Dec 20 2007
A team of investigators from the Massachusetts General Hospital (MGH) Biomicroelectromechanical Systems (BioMEMS) Resource Center and the MGH Cancer Center has developed a microchip-based device that can isolate, enumerate and analyze circulating tumor cells (CTCs) from a blood sample. CTCs are viable cells from solid tumors carried in the bloodstream at a level of one in a billion cell. Because of their rarity and fragility, it has not been possible to get information from CTCs that could help clinical decision-making, but the new device – called the “CTC-chip,”– has the potential to be an invaluable tool for monitoring and guiding cancer treatment.
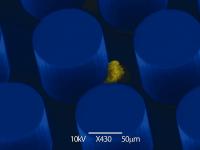 Scanning electron microscope image of a lung cancer cell adhering to an antibody-coated micropost on the CTC-chip.
Scanning electron microscope image of a lung cancer cell adhering to an antibody-coated micropost on the CTC-chip.
“This use of nanofluidics to find such rare cells is revolutionary, the first application of this technology to a broad, clinically important problem,” says Daniel Haber, MD, director of the MGH Cancer Center and a co-author of the report in the December 20 issue of Nature. “While much work remains to be done, this approach raises the possibility of rapidly and noninvasively monitoring tumor response to treatment, allowing changes if the treatment is not effective, and the potential of early detection screening in people at increased risk for cancer.”
The existence of CTCs has been known since the mid-19th century, but since they are so hard to find, it has not been possible to adequately investigate their biology and significance. Microchip-based technologies have the ability to accurately sense and sort specific types of cells, but have only been used with microliter-sized fluid samples, the amount of blood in a fingerprick. Since CTCs are so rare, detecting them in useful quantities requires analyzing samples that are 1,000 to 10,000 times larger.
To meet that challenge the MGH BioMEMS Resource Center research team – led by Mehmet Toner, PhD, senior author of the Nature report and director of the center in the MGH Department of Surgery, and Ronald Tompkins, MD, ScD, chief of the MGH Burns Unit and a co-author – first investigated the factors required for microchip analysis of sufficiently large blood samples. The device they developed utilizes a business-card-sized silicon chip, covered with almost 80,000 microscopic posts coated with an antibody to a protein expressed on most solid tumors. The researchers also needed to calculate the correct speed and force with which the blood sample should pass through the chip to allow CTCs to adhere to the microposts.
“We developed a counterintuitive approach, using a tiny chip with critical geometric features smaller than a human hair to process large volumes of blood in a very gentle and uniform manner – almost like putting a ‘hose’ through a microchip,” explains Toner.
Several tests utilizing cells from various types of tumors verified that CTCs were captured by posts covered with the antibody ‘glue.’ Even tumor cells expressing low levels of the target protein and samples containing especially low levels of CTCs were successfully analyzed by the CTC-chip. In contrast to current technology for detecting CTCs, the new microchip device does not require any pre-processing of blood samples, which could damage or destroy the fragile CTCs.
The researchers then tested the CTC-chip against blood samples from 68 patients with five different types of tumors – lung, prostate, breast, pancreatic and colorectal. A total of 116 samples were tested, and CTCs were identified in all but one sample, giving the test a sensitivity rating of 99 percent. No CTCs were found in samples from cancer-free control volunteers. To evaluate the device’s ability to monitor response to treatment, blood samples were taken from nine cancer patients during their treatment for lung, colorectal, pancreatic or esophageal tumors. Changes in levels of CTCs accurately reflected changes in tumor size as measured by standard CT scans.
“We looked at four major cancer killers and were able to consistently find these cells and correlate test results with traditional monitoring techniques,” Toner says. “Some of these tumors have several potential drugs to choose from, and the ability to monitor therapeutic response in real time with this device – which has an exquisite sensitivity to CTCs – could rapidly signal whether a treatment is working or if another option should be tried.”
CTCs also can provide the molecular information needed to identify tumors that are candidates for the new targeted therapies and should help researchers better understand the biology of cancer cells and the mechanisms of metastasis. Considerable work needs to be done before the CTC-chip is ready to be put to clinical use, and the MGH investigators are establishing a Center of Excellence in CTC Technologies to further explore the potential of the device, which also has been licensed to a biotechnology company for commercial development.