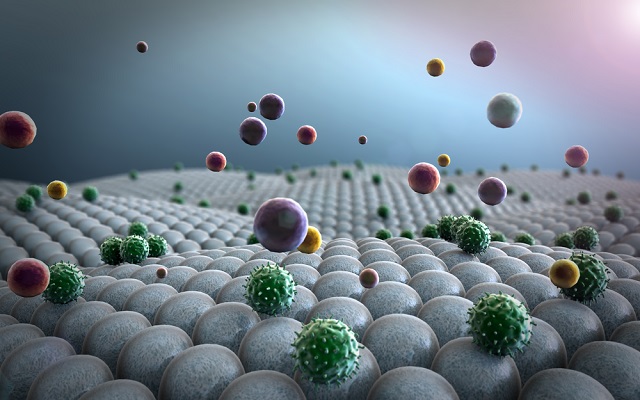
A nanoparticle drug delivery system for the treatment of pneumonia has been developed. An active drug is trapped inside the nanoparticles, which only release the drug when they have been absorbed by immune cells. This method increases the drugs potency whilst reducing any harmful or unpleasant side-effects it may cause.
UGREEN 3S | Shutterstock
When using the new nanoparticle system to deliver antibiotics its effectiveness against pneumonic tularaemia is greatly enhanced. Pneumonic Tularaemia, a form of pneumonia, is caused by the inhalation of the bacterium Francisella tularensis.
The mesoporous silica nanoparticles that were used in the drug delivery system were developed by Jeffrey Zink at UCLA. Zink, along with his team, has conducted extensive research to determine the right particle to use to optimise drug delivery system.
The nanoparticles are full of deep empty pores. We place the particles in drug solution overnight, filling the pores with drug molecules. We then block the pore openings on the nanoparticle’s surface with molecules called nanovalves, sealing the drug inside the nanoparticle.
Jeffrey Zink - UCLA
The research involved injecting an infected mouse with nanoparticles saturated with the drug. The drug remains in the nanoparticles and are carried through the mouse's body until they reach their target, which are macrophages; a type of white blood cell.
The nanoparticles are taken up by the macrophages and introduced to their acidic environment. The nanovalves, which are triggered to open by acid, then release the drug.
We tested several different particles and nanovalves until we found the ones that would carry the maximum amount of drug and release it at just the right pH value.
Jeffrey Zink - UCLA
The Centers for Disease Control has declared the highly infectious F. tularensis bacterium as a top-tier bioterrorism agent, implying that it is a great risk to public health and national security.
F. tularensis survives and multiplies within macrophages, especially those in the liver, spleen and lung. Macrophages readily devour mesoporous silica nanoparticles, making these particles ideal for treating these types of infections.
Marcus Horwitz - UCLA
Although moxifloxacin is a powerful drug for the treatment og tularaemia, it causes significant side effects when administered directly into the blood stream as a free drug. The research team strived to maximize its efficiency whilst reducing the side effects.
When you give a drug freely in the blood, only 1 or 2 percent of it gets to where you want it to go. With this system, the drug is contained inside the nanoparticles until they are inside macrophages, delivering a much larger amount of the drug directly to the site of infection.
Marcus Horwitz - UCLA
According to Horwitz, freely injected drugs are metabolised and get expelled, a process which begins immediately following administration. Using nanoparticles prevent drugs from being metabolised and excreted until after they are released in the target cells.
The efficiency of freely administered moxifloxacin was compared with its efficiency when delivered using nanoparticles. Delivery of moxifloxacin through nanoparticles into mice with a high dose of Francisella tularensis was far more effective with less side effects.
The nanoparticle drug delivery system resulted in a significant decrease in the number of bacteria present in the lungs, which was much higher than that achievable by a four times greater dose of freely injected moxifloaxin.
The research findings have been published in the journal ACS Nano.