Spatiotemporal delivery of nanoparticles at the cellular level is desirable in nanomedicine to deliver a maximum cytotoxic drug into cancer cells via the accumulation of the nanoparticles in tumors. Nevertheless, the cancer-associated fibroblasts (CAFs) and macrophages in tumor cells reduce the efficiency of nanoparticle delivery in the spatiotemporal region.
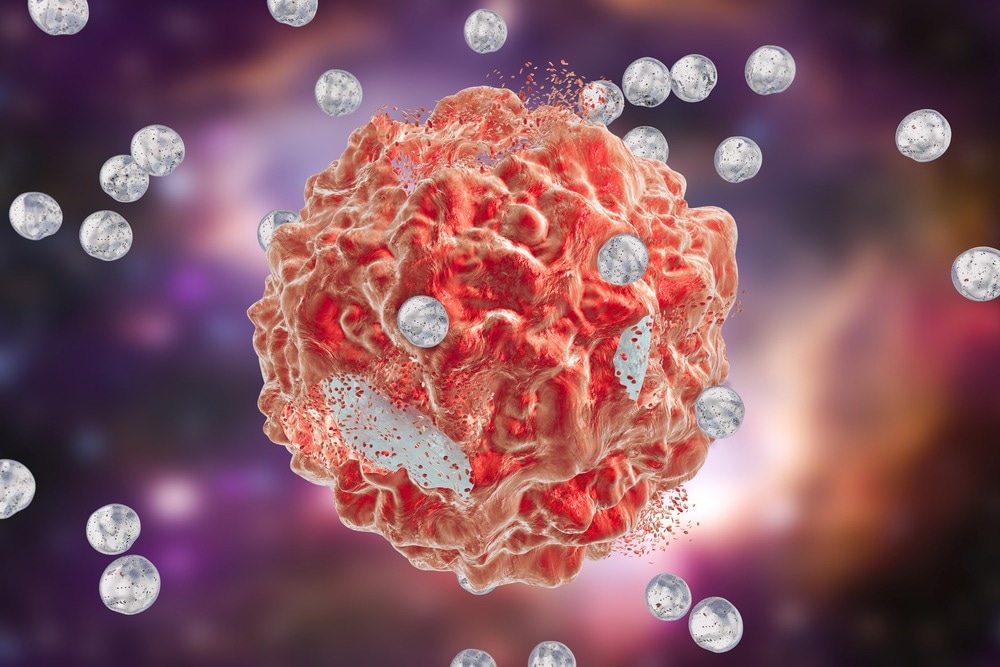
Study: Glutathione Pulse Therapy: Promote Spatiotemporal Delivery of Reduction-Sensitive Nanoparticles at the “Cellular Level” and Synergize PD-1 Blockade Therapy. Image Credit: Kateryna Kon/Shutterstock.com
In an article published in the journal Advanced Science, glutathione (GSH) pulse therapy based on a reduction-sensitive larotaxel (LTX) prodrug was developed as a nanoparticle delivery system for tumor cells. These nanoparticle delivery systems escaped the phagocytosis of macrophages and facilitated the penetration through the CAF-induced stromal barrier, as observed in an animal model with breast cancer.
Along with improving the penetration of these nanoparticle delivery systems into tumor cells, this therapy also helped in LTX accumulation in cancer cells and refurbished the immunosuppressive microenvironment to combine PD-1 blockade therapy. Moreover, the biodistribution of the designed nanoparticle delivery systems could be analyzed by quantifying their in vivo biodistribution between different cells.
Nanoparticle Delivery Systems for Anticancer Therapy
Nanoparticles of therapeutic potency have specific sizes, shapes, and surface characteristics that primarily influence the efficiency of nanoparticle delivery systems and thus control therapeutic efficacy. Nanoparticles with a diameter range between 10 and 100 nanometers are suitable for cancer therapy, as they can effectively deliver drugs.
Smaller nanoparticles (1 to 2 nanometers) can easily leak from the normal vasculature to damage normal cells and are easily filtered by kidneys (less than 10 nanometers in diameter), while the nanoparticles that are larger than 100 nanometers are likely to be cleared from circulation by phagocytes.
With the increasing importance of nanomedicine in cancer therapy, many nanoparticle delivery systems have been approved by the United States Food and Drug Administration (USFDA). Specifically, spatiotemporal nanoparticle delivery systems were applied to cancer treatment, and their therapeutic efficiency depends on the biodistribution of agents in spatial and temporal regions in tumor cells.
Macrophages in the tumor microenvironment (TME) affect the accumulation of nanoparticle delivery systems in spatiotemporal regions since most of the delivered nanoparticles are engulfed by them. Thus, phagocytosis of macrophages in the TME nullifies the therapeutic effects of nanoparticle delivery systems in tumor tissue.
Consequently, the spatiotemporal accumulation of nanoparticle delivery systems restricted at the tumor tissue level is insufficient to exhibit therapeutic efficiency and requires advancement to the cellular level, focusing on delivering a cytotoxic drug into cancer cells.
To this end, various nanoparticle delivery systems based on liposomes, polymeric nanoparticles, polymeric micelles, polymer-drug conjugate nanoparticles, and lipid-drug conjugate nanoparticles have been developed to date. While a few of these are under preclinical or clinical trials, others are on the market.
Glutathione Pulse Therapy Using Nanoparticle Delivery Systems
Based on previous studies, the authors hypothesized that GSH injections could positively impact the immune-suppressive and tumor-stromal microenvironment induced by CAFs and benefits the PD-1/PD-L1 checkpoint inhibitor therapy.
Thus, to test this hypothesis, three different nanoparticle delivery systems based on reduction-sensitive LTX prodrug nanoparticles with α, β, and γ disulfide bonds were designed and synthesized. Subsequently, the GSH pre-injections and injections based on therapeutic outcomes in murine triple-negative breast cancer models with a maximum accumulation of the LTX prodrug nanoparticles, termed GSH pulse therapy, were investigated.
Moreover, to observe the changes of cumulative drugs at the cellular level, a sophisticated method was established, wherein matrix-assisted laser desorption/ionization mass spectrometry imaging (MALDI-MSI), flow cytometry and cell sorting (FACS), and confocal laser scanning microscopy technologies were used to quantify the amount of drug delivered in target cells.
While MALDI-MSI imaging technology could map the biodistribution of drugs within the tissue, combining this method with a confocal microscope helped observe the changes in the LTX and LTX-SS-CA prodrugs distribution among macrophages and cancer cells.
Furthermore, combining FACS with liquid chromatography with tandem mass spectrometry (LC-MS/MS) helped quantify the accumulation of drugs in both macrophages and cancer cells. Fluorescent protein-based sophisticated transfection technology ensured the segregation of every cell type by FACS. Thus, the present study is suitable to investigate the biodistribution of nanoparticle delivery systems and antibody-drug conjugates (ADCs) at the cellular level required for advanced nanomedicine.
Conclusion
Overall, nanoparticle delivery systems, unlike conventional therapeutics, have the advantage of easy designing and tuning to reach the target site, not only to treat cancer but many other diseases. The GSH pulse therapy developed in the present study enables the reduction-sensitive nanoparticles to deliver the drugs to spatiotemporal regions of cancer cells that could synergize PD1 blockade therapy.
Subsequently, an analytical method that helped study the distribution of nanoparticle delivery systems at the cellular level included the integration of the FACS, MADLI-MSI, and confocal microscope technologies. Moreover, the established method was not only suitable for nanoparticle delivery systems but also ADCs and other targeted biomaterials.
Reference
Dong, S., Zhang, Y., Guo, X., Zhang, C., Wang, Z., Yu, J., Liu, Y et al. (2022) Glutathione Pulse Therapy: Promote Spatiotemporal Delivery of Reduction-Sensitive Nanoparticles at the “Cellular Level” and Synergize PD-1 Blockade Therapy. Advanced Sciences. https://onlinelibrary.wiley.com/doi/10.1002/advs.202202744
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.