Glioblastoma (GBM) is the most common and highly malignant cancer in the adult brain, characterized by poor prognosis and aggressive infiltration. A long-standing problem in GBM treatment is the delivery of therapeutics to brain-invading tumor cells that is obstructed by the blood−brain barrier (BBB). Immune checkpoint blocker-based combination therapy stands critical for GBM treatment.
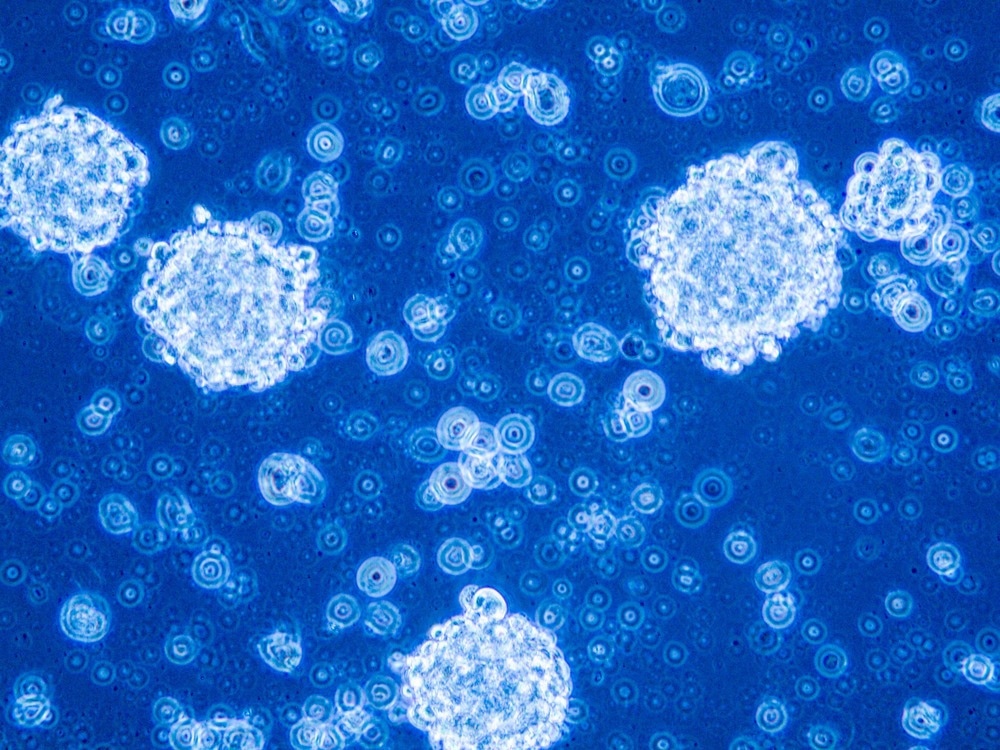
Study: Engineered Macrophage-Membrane-Coated Nanoparticles with Enhanced PD-1 Expression Induce Immunomodulation for a Synergistic and Targeted Antiglioblastoma Activity. Image Credit: Anna Durinikova/Shutterstock.com
In an article published in the journal Nano Letters, a macrophage membrane-coated nanoplatform was engineered with the expression of programmed cell death-1 (PD-1) (PD-1-MM@PLGA/RAPA) that was effective in crossing the BBB in response to the tumor microenvironment (TME) recruitment, facilitating the accumulation of nanoparticles at the target site.
An enhanced immune response was observed due to improved CD8+ cytotoxic T-lymphocyte (CTL) infiltration. Thus, the engineered robust nanoplatform served as an efficient tool for combinational chemotherapy against a wide range of cancers.
Nanoparticles for GBM Therapy
GBM is an aggressive type of primary brain cancer, with a median survival of 12 months from the initial diagnosis. These invasive glioma cells can migrate extensively into the brain and are often resistant to therapy. Thus, GBM has a high level of reoccurrence and mortality. Collectively, the location and reoccurrence of GBM restrict the improvement in prognosis.
Tumor-associated macrophages (TAMs) represent a significant part of the non-neoplastic cell population within the glioma TME. TAMs express an M2-like phenotype in GBM, endowing immunosuppressive functionalities in TAMs, enabling them to orchestrate tumor growth and invasiveness.
PD-1/programmed cell death ligand 1 (PD-L1) is critical for molecular connections among GBM cells, TAMs, and tumor-infiltrating T lymphocytes (TILs). PD-L1 is overexpressed in TAMs and tumor cells. It binds to PD-1 that expresses TIL, inducing T cell depletion and apoptosis, and suppresses the activation of CTL, facilitating the tumor cell’s escape from the immune system. Consequently, PD-1/PD-L1 immune checkpoint blockade is effective in CTL-mediated immune killing.
Drug delivery systems based on nanoparticles can overcome the limitations of conventional chemotherapy by improving systemic biodistribution, increasing drug circulatory half-life, and enhancing intracellular trafficking. Additionally, physiochemical properties and surface profiles of nanoparticles can be engineered with molecular ligands, enabling tumor-specific targeting.
Therapeutic nanoparticles can control drug release kinetics, reducing the need for multiple administrations. Furthermore, nanoparticles can be formulated with multiple drugs for combination therapies. The physicochemical properties of nanoparticles dictate their ability to transport across or circumvent the BBB.
Engineered Macrophage-Membrane-Coated Nanoparticles for Anti-GBM Activity
Recently, natural cell membrane-based nano drug delivery systems were explored for their TME response and BBB penetrating ability. Natural cell membranes derived from neutrophils, macrophages, erythrocytes, endothelial cells, platelets, and mesenchymal stem cells were extensively used in theranostic research to target TME in tumor cells.
Moreover, previous reports indicated macrophage’s response to the GBM microenvironment, implying the ability of macrophage membrane to provide nanoparticles with the drug delivering ability over BBB based on their response to TME.
In the present work, PD-1-MM@PLGA/RAPA nanoplatforms were engineered based on macrophage-membrane-coated nanoparticles with the ability to cross the BBB, exhibiting TME-based response, and PD-1/PD-L1 signal axis targeting ability.
Although previous reports mentioned the ability of macrophages to express PD-1, these were unregulated in terms of TME-based response and pathogen infection. Moreover, lipopolysaccharide-stimulated macrophages showed 3.89-fold more PD-1 microRNA expression than unstimulated cells.
In the current work, a genetic engineering strategy was adopted to enhance the PD-1 expression within the macrophages by their transduction with vectors, encoded with the PD-1 gene, infected with lentivirus, tagged with copepod green fluorescent protein, and screened with puromycin [LV2 CMV-EF1α-cGFP(2A)-Puro].
Real-time quantitative polymerase chain reaction (RT-qPCR) helped confirm a 173-fold enhanced PD-1 microRNA expression in engineered macrophages (RAW 264.7-PD-1) compared to their non-engineered counterparts (RAW 264.7), suggesting the robustness of the adopted strategy.
Furthermore, in vitro and in vivo studies were performed to elucidate immune checkpoint
blockade (ICB) mechanisms of the constructed chemotherapeutic-targeted delivery system. The in vitro studies revealed the antitumor efficiency of PD-1-MM@PLGA/RAPA nanoparticles.
Here, animal models treated with PD-1-MM@PLGA/RAPA nanoparticles showed a high level of tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ), indicating the efficiency of PD-1-MM@PLGA/RAPA nanoparticles in exerting an anti-GBM effect. The in vivo study on the C6-luc GBM tumor model using PD-1-MM@PLGA/RAPA nanoparticles confirmed their antineoplastic efficiency with extended survival time.
Conclusion
To summarize, PD-1-MM@PLGA/RAPA nanoparticles were designed and applied as a therapeutic strategy to treat GBM. The macrophage-membrane-coated nanoparticles were potent in crossing the BBB and reaching the brain in response to TMA-based chemokines.
The PD-1/PD-L1 signal axis blockade helped PD-1-MM@PLGA/RAPA nanoparticles to target the PD-L1 and achieve the anti-GBM therapeutic effect. Subsequently, TILs and CTLs are activated at the tumor site, triggering cytokines release and antitumor effect.
Compared to the non-engineered cell-membrane-coated nanoparticles, their engineered counterparts served as better drug delivery nanoplatform in achieving in vivo anti-GBM effect due to enhanced PD-1 expression.
Reference
Yin, T., Fan, Q., Hu, F., Ma, X., Yin, Y., Wang, B., Kuang, L et al. (2022). Engineered Macrophage-Membrane-Coated Nanoparticles with Enhanced PD-1 Expression Induce Immunomodulation for a Synergistic and Targeted Antiglioblastoma Activity. Nano Letters. https://pubs.acs.org/doi/10.1021/acs.nanolett.2c01863
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.