In a healthy brain, the blood-brain barrier (BBB) serves as a diffusion barrier that is essential for protecting normal brain function by impeding the entry of most compounds from the blood to the brain. Consequently, despite the efficiency of brain-targeting therapeutic oligonucleotides in treating several brain illnesses, the BBB restricts their transport effectiveness to the brain.
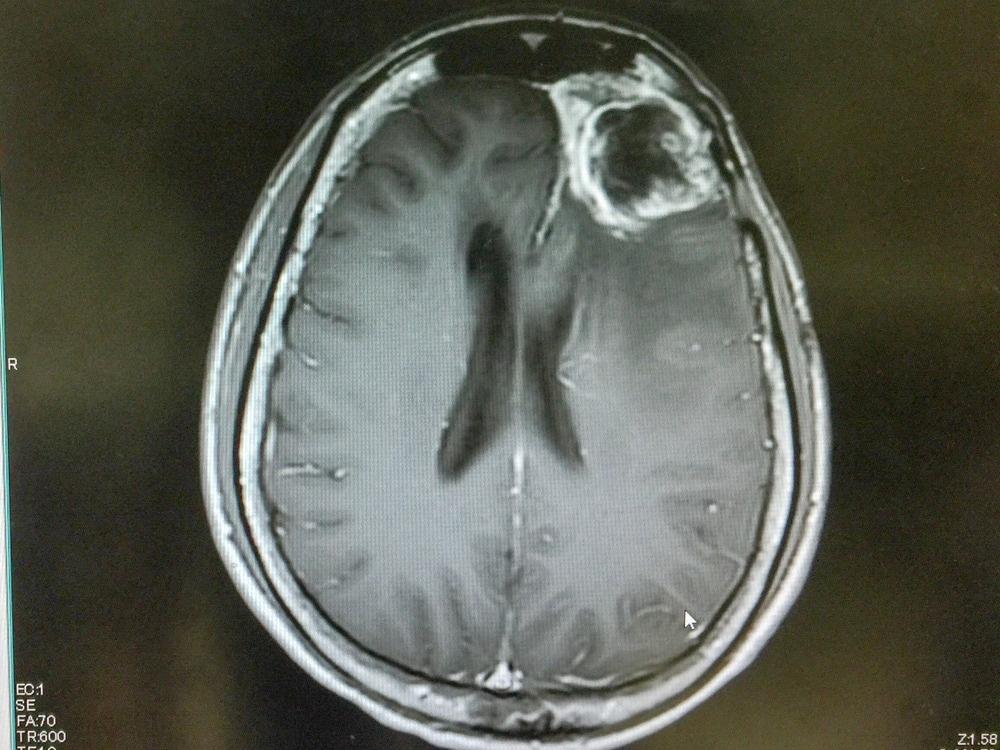
Study: Brain-targeted exosome-mimetic cell membrane nanovesicles with therapeutic oligonucleotides elicit anti-tumor effects in glioblastoma animal models. Image Credit: O_Akira/Shutterstock.com
An article published in Bioengineering and Translational Medicine presents cell membrane nanovesicles that mimic natural exosomes to improve therapeutic oligonucleotide’s targeted delivery into the brain.
Cell membrane nanovesicles were isolated from C6 cell membrane fragments via extrusion and coated with T7 peptides, producing a targeting ligand, T7-cell membrane nanovesicles. The size of prepared nanovesicles was maintained in an aqueous solution for over 21 days. Furthermore, the efficiency of the targeted delivery of T7-cell membrane nanovesicles was evaluated using a glioblastoma animal model.
2′-O-methyl and cholesterol-TEG-modified anti-microRNA-21 oligonucleotides (AMO21c) were loaded into T7-cell membrane nanovesicles. Biodistribution tests indicated that the T7-cell membrane nanovesicles carried AMO21c into the brain more efficiently than scrambled T7-cell membrane nanovesicles, pure-cell membrane nanovesicles, naked AMO21c, and lipofectamine, following their systemic administration.
Furthermore, in the T7-cell membrane nanovesicles group, AMO21c efficiently down-regulated the levels of miRNA-21 in glioblastoma tissues, leading to the upregulation of PTEN and PDCD4. Compared to other control groups, the brain tumor size was reduced in the T7-cell membrane nanovesicle groups. With low toxicity, stability, and targeting efficiency, T7-cell membrane nanovesicles may be useful for developing oligonucleotide therapies for brain tumors.
Therapeutic Strategies for Glioblastoma
Glioblastoma is the most common primary brain tumor. The blood-brain tumor barrier (BBTB) permeability in glioblastomas is high in bulk tumor areas but slight or null in peripheral regions. Thus, combining the BBB and BBTB forms a major barrier to brain tumor drug delivery.
Gene therapy has been well-researched as a novel therapeutic option for the treatment of glioblastoma. Preclinical and clinical studies on the herpes simplex virus thymidine kinase (HSVtk) gene as a therapeutic target for glioblastoma have revealed its beneficial impact.
However, clinical trials employing HSVtk gene therapy, in conjunction with chemotherapy and radiation, have shown unsatisfactory results. Small interfering RNAs (siRNAs) and antisense oligonucleotides have been studied for use in glioblastoma gene therapy.
Previous studies have suggested that oncogenic miRNAs play key roles in the development of cancers, including glioblastoma. Some miRNAs are upregulated in tumor tissues and promote tumor cell proliferation and survival. Additionally, administration of the anti-miRNA-21 oligonucleotide (AMO21) reduced miRNA-21 levels and expression of PDCD4 and PTEN in tumor tissues. Consequently, tumor cell growth is suppressed, triggering apoptosis.
Brain Tumor-Targeting Exosome-Mimetic Cell Membrane Nanovesicles
In this study, T7-cell membrane nanovesicles targeting the brain tumor were developed and evaluated as AMO21 nanocarriers. In vivo and in vitro studies have suggested that the prepared brain tumor-targeting nanovesicles deliver AMO21c into brain tumor cells and inhibit their growth by suppressing the expression of miRNA-21.
Despite extensive efforts to develop drug delivery systems based on cell membrane nanovesicles, nucleic acid drug delivery through these systems has not been attempted. Moreover, exosome-assisted delivery of AMOs has been reported to have few obstructions owing to inefficient loading.
In this study, AMO21c was loaded onto T7-cell membrane nanovesicles via hydrophobic interactions between the cell membranes and cholesterol. The in vivo, and in vitro toxicity assays confirmed the biosafety of AMO21c, suggesting that cholesterol-linked AMO21c may not induce toxicity. Therefore, chemical modification of AMO21 minimized AMO21c degradation.
Although previous studies have mentioned the interference of AMO21c on the surface of cell membrane nanovesicles in targeting T7 peptides, the in vivo results here revealed the efficiency of T7-cell membrane nanovesicles in delivering AMO21c into glioblastoma tissue.
Cell membrane nanovesicles derived from tumor cell membranes have been demonstrated to exhibit tumor-targeting properties by previous researchers. In addition, T7 peptide-decorated cell membrane nanovesicles have enhanced brain transport efficiency. This implies that decorating targeting ligands on tumor cell membrane-coated nanoparticles or other forms of cell membrane nanovesicles may have comparable effects on the delivery efficiency.
It has been previously proposed that cell membrane nanovesicles exhibit exosome-like features, including the ability to penetrate the BBB. However, the distribution efficiency can be improved by utilizing targeted ligands.
Conclusion
In summary, the present study developed glioblastomas targeting cell membrane nanovesicles decorated with targeting ligands. T7-cell membrane nanovesicles carry AMO21c across the BBB into glioblastoma tissues following intravenous injection.
As a result, increased AMO21c delivery reduced miRNA-21 levels, resulting in the recovery of genetic markers. T7-cell membrane nanovesicle/AMO21c therapy considerably decreased overall cancer size. These findings suggested that T7-cell membrane nanovesicles may be effective carriers for delivering AMO21c to treat glioblastoma.
Reference
Lee, Y, Kim, M, Ha, J, Lee, M. (2022). Brain-targeted exosome-mimetic cell membrane nanovesicles with therapeutic oligonucleotides elicit anti-tumor effects in glioblastoma animal models. Bioengineering and Translational Medicine. https://doi.org/10.1002/btm2.10426
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.