A new approach to brain tumor treatment using photodynamic therapy (PDT) with nanotechnology has been explored in a review published in the journal Biomedicines. Unlike radiotherapy and surgical resection, PDT can treat micro-invasive areas and protect critical brain tissue with a high probability of success.

Study: Nanomedicine in Clinical Photodynamic Therapy for the Treatment of Brain Tumors. Image Credit: peterschreiber.media/Shutterstock.com
Conventional Methods using PDT
Photodynamic therapy is a type of phototherapy that uses light and sensitizing chemical agents in combination with oxygen molecules to induce cell death. It is a two-stage remedy that incorporates light energy with a medicine (photosensitizer) designed to kill cancer cells and precancerous cells after they have been activated by light.
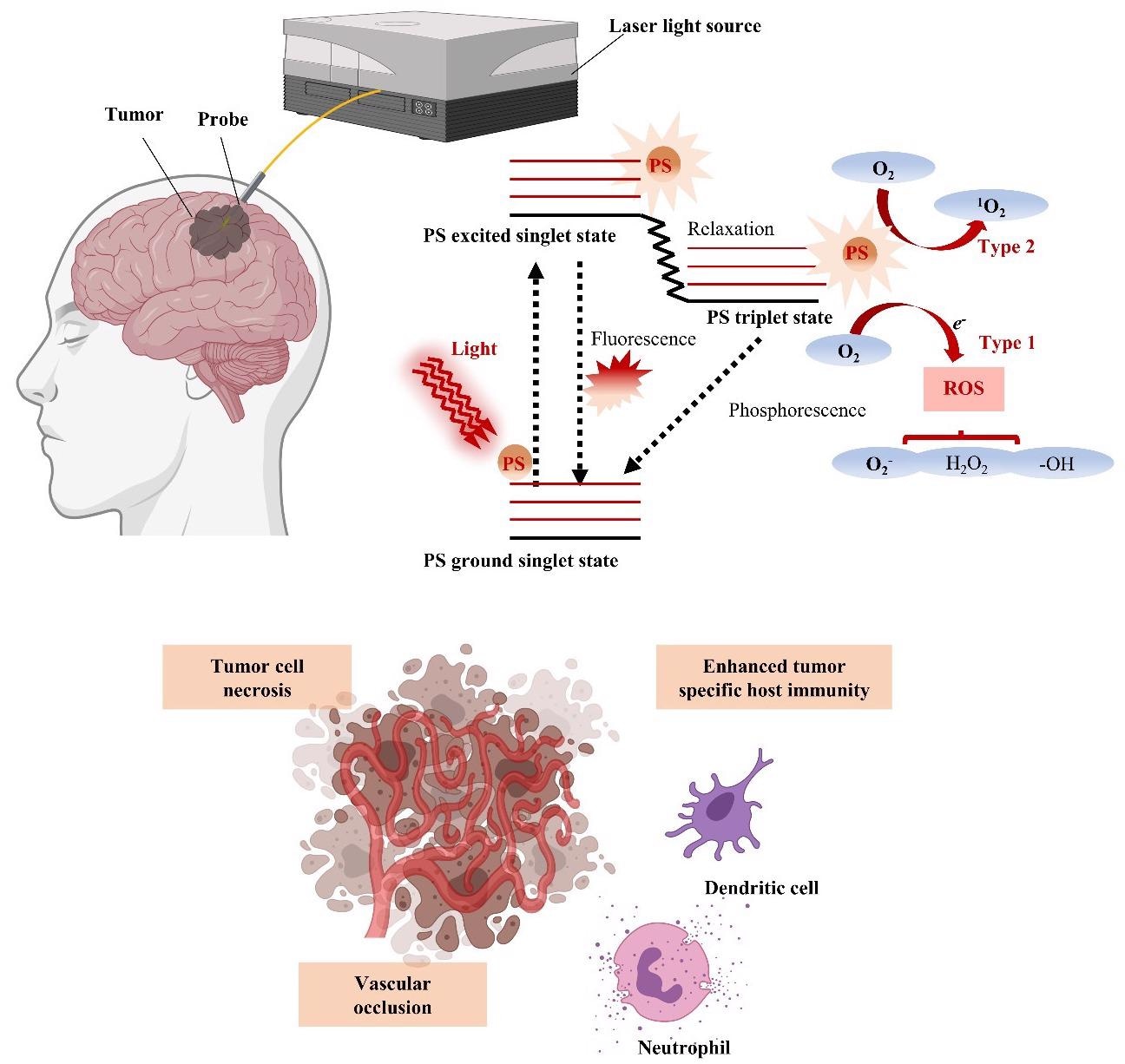
Schematic illustration of photodynamic therapy (PDT) for GBM treatment with energy diagram of the oxygen dependent response. If the photosensitizer (PS) in the ground singlet state is excited by the light wavelength, then the PS in the excited singlet state can convert to the excited triplet state via intersystem crossing. In the presence of molecular oxygen, the PS in the triplet state can undergo a Type 1 or Type 2 redox reaction, producing reactive oxygen species (ROS) that cause tumor cell necrosis, vascular occlusion, and tumor-specific host immunity. © Kim, H., and Lee, D. (2022).
Photosensitizers are initiated by a specific wavelength energy, which is typically generated by a laser. PDT has been shown to be effective in treating a variety of tumors, including melanoma, squamous cell carcinoma, and multidrug-resistant lung and mammary tumors.
PDT with Its Limited Efficacy
Following other oncology implementations, the interest in PDT as a high-grade glioma diagnosis stems from the essence of tumor growth and the limited efficacy of modern treatment options to this population of patients. Although surgical removal, partial radiation, and chemotherapy are important treatments for intracranial tumors, the obtrusive growth patterns, especially in the cerebrum's central region, make total resection difficult.
As opposed to surgical resection and radiation, PDT can treat micro-invasive regions while preserving sensitive brain areas. These potential benefits over conventional therapies have been shown to improve results in clinical situations with low overall survival and a high incidence of iatrogenic damage.
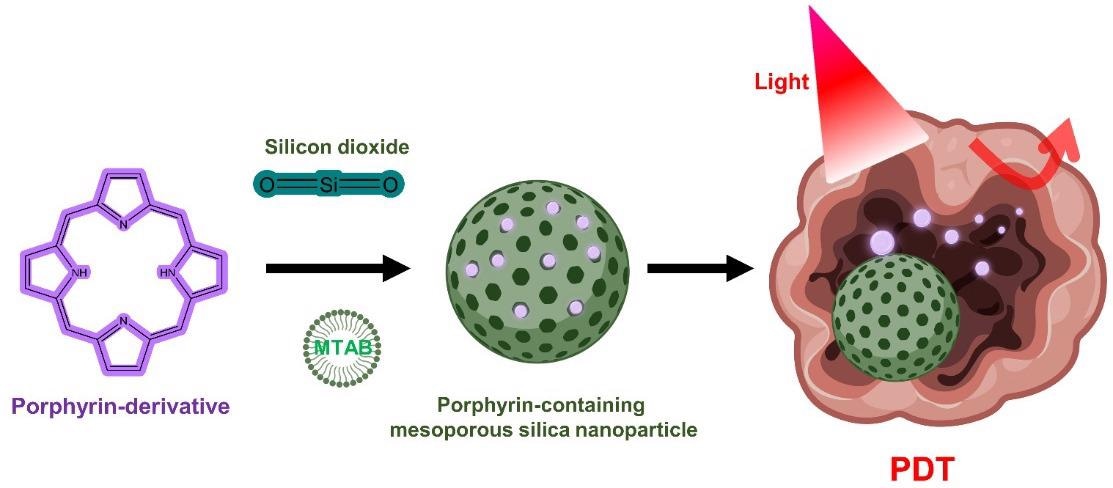
Porphyrin-containing mesoporous silica nanoparticles for PDT. © Kim, H., and Lee, D. (2022).
Nanomedicine as Opposed to Conventional Method
The rapidly growing areas of nanotechnology and nanomedicine are yielding nanostructured materials that may overcome the limitations of conventional clinical delivery methods. In fact, the existence of a functioning blood–brain barrier (BBB) inhibits therapeutic delivery to brain malignancies.
Many ways for temporarily opening the BBB by physical impact, including magnetic resonance (MR)-guided focussed ultrasound, have lately been researched to circumvent this barrier; however, this poses a technical problem.
One of the most promising solutions involves the utilization of multifunctional nanomedicines as drug delivery systems.
Advantages of Nanomedicine
The excellent physical and mechanical characteristics of nanocarriers vary based on their material, size, form (mesoporous microstructure, rod shape, particles), and ligand of choice. This enables enhanced brain-targeted administration of PS or therapeutic medicines.
Although many PS nanocapsules are still in the early phases of translation, major improvements in functional nanomedicines relying on BBB crossing have been accomplished in recent years.
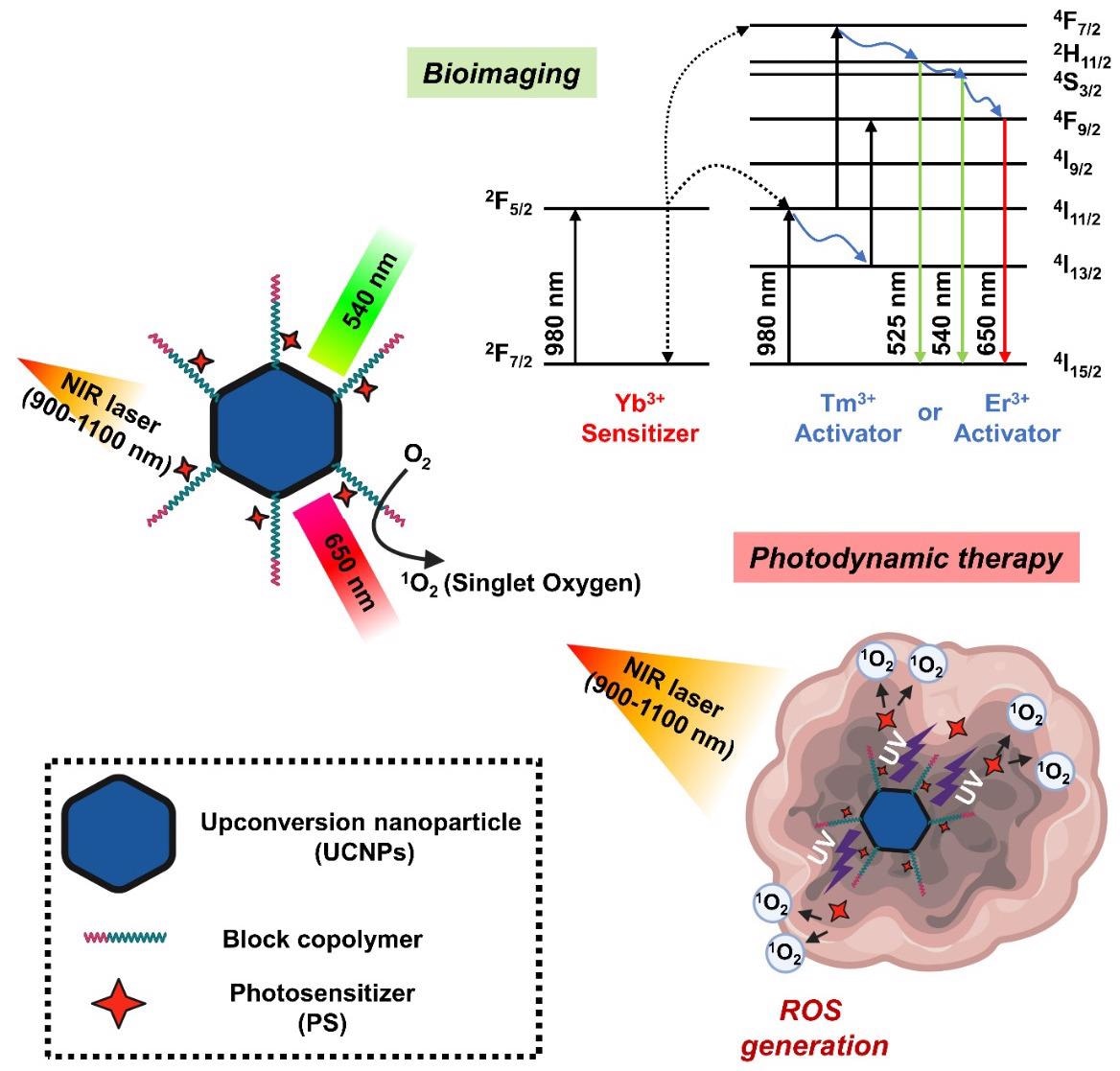
Schematic diagram showing the mechanism of photodynamic therapy and bioimaging through long-wavelength to short-wavelength conversion of upconversion nanoparticles (UCNPs). © Kim, H., and Lee, D. (2022).
Another benefit of nanoparticles is that they may boost PS's poor solubility, extend blood circulation, promote the targeted distribution and cellular absorption, and protect the medication from degradation.
Nanoparticles in PDT for Healing
Although contemporary PDT has considerably improved cancer patients' quality of life and survival rates, it is critical to further enhance the therapeutic efficacy of nanocarriers to eliminate noticeable side effects.
In this respect, researchers have investigated a variety of nanocarriers, including polymers, liposomes, micelles, inorganic oxide, and new metal nanoparticles, to improve the therapeutic efficiency of photosensitizers.
First and foremost, nanocarriers must be used to effectively transport photosensitizers and singlet oxygen molecules to the target region in an ideal therapeutic range.
PDT is a dynamically evolving profession that is continually on the lookout for innovative technologies. To improve the efficacy and selectivity of PDT, molecular techniques based on nanotechnology are being explored. As a result, several novel organic and inorganic nanoparticles have already been discovered and produced for the targeted administration of photosensitizer medicines.
Nanoparticles may remedy the significant constraints of standard PS medication delivery.
Limitation of this Nanotechnology PDT
However, since intracranial brain tumors emerge from complex structures and distinct organs, such as those bordered by the blood–brain barrier, it is questionable if they can be completely removed using the same strategy as other cancers.
Further research is needed to determine if PDT may be utilized to treat malignant brain cancer that cannot be removed due to its location.
Ongoing research into the numerous PDTs described in this publication will decide whether breakthroughs in cancer research can reduce morbidity and mortality from intracranial malignancy and have the potential to change brain tumor therapy. As a result, although the development of new PDT technology is critical, establishing therapeutic guidelines via large-scale clinical practice should be prioritized.
Future Research in this Nanomedicine to Cure Brain Cancer
With the fast advancements in nanotechnology, researchers now have several synthetic approaches at their disposal to create gold nanoparticles with good shapes and characteristics for PDT applications.
In addition to the numerous physicochemical qualities listed above, the extra various synthesis potential should increase bioavailability and usefulness, indicating gold nanoparticles as a suitable choice for therapeutic cancer therapy.
Continue reading: Detecting Lung Cancer Early with Non-Invasive Nanosensors.
Reference
Kim, H., and Lee, D. (2022). Nanomedicine in Clinical Photodynamic Therapy for the Treatment of Brain Tumors. Biomedicines 2022, 10(1), 96. Available at: https://www.mdpi.com/2227-9059/10/1/96/htm
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.