Studying tumor physiology entails a better understanding of the complex interactions between tumors and their surrounding microenvironments.1 A better comprehension of cancer biology is crucial for developing effective diagnostics and treatments for different types of cancer. This article focuses on how the application of nanoscale tools has revolutionized tumor physiology research.
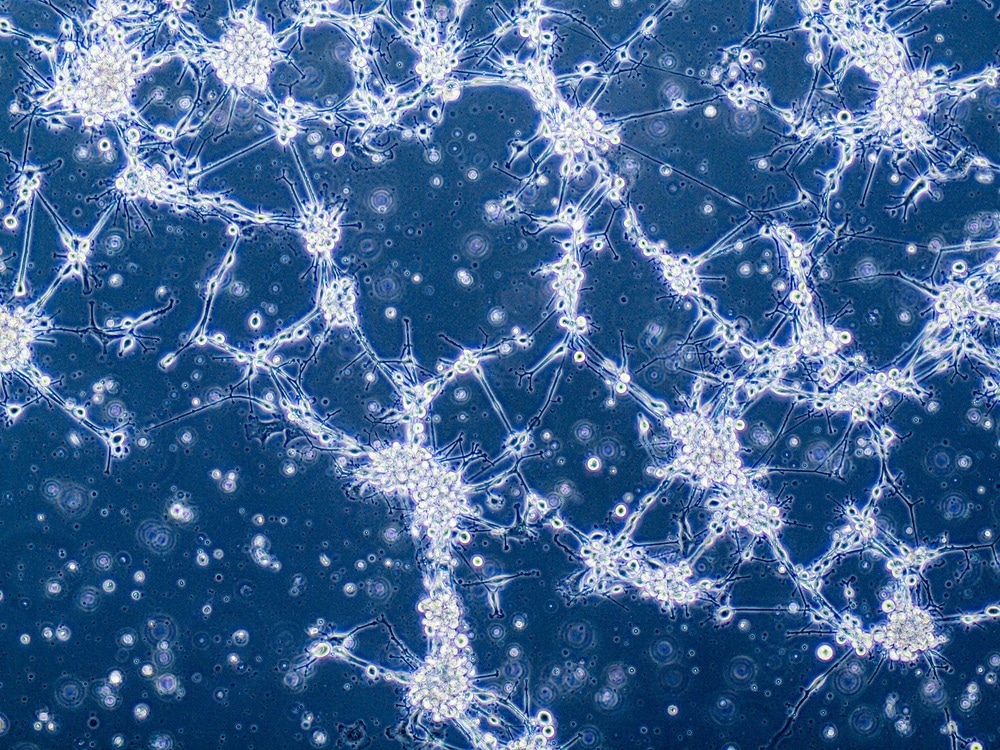
Image Credit: Anna Durinikova/Shutterstock.com
Introduction to Tumor Physiology
A tumor is a solid mass of tissue that forms due to abnormal cell growth. Tumors are of two types, namely, benign and malignant. In contrast to a malignant tumor or cancer, a benign tumor is associated with abnormal cell growth that does not spread or invade adjacent tissues or other body parts.2 It is difficult to detect tumor cells because of their metastatic and invasive nature.
Tumor physiology describes the innumerable physiological changes that lead to alterations in the immune system, cancer cell invasion and spread, and changes in metabolic pathways. Angiogenesis is a key feature of tumor physiology, which entails the formation of new blood vessels in the growing tumor mass. These new blood vessels supply oxygen and nutrients to the tumor cells, essential for their growth.3
Tumor cells trigger angiogenesis by activating growth factors that lead to the development of new blood vessels. Scientists involved in cancer research are focused on understanding the process and mechanism underlying angiogenesis as it plays a key role in cancer progression.
Besides angiogenesis, tumor physiology also describes how the immune system responds to cancer cells.4 Many studies have highlighted that tumor cells escape immune surveillance by downregulating major histocompatibility complex (MHC) expression. The main function of MHC is to help the immune system recognize foreign substances.5
As stated above, the tumor microenvironment (TME) shapes the progression of cancers through the interaction between the tumor cells and adjacent stroma cells. Besides TME, endothelial cells and tumor-associated macrophages (TAM) are primary components that determine cancer progression, metastasis formation, and therapy resistance.6
Why are Nanoscale Tools Used to Study Tumor Physiology?
Nanoparticles (NPs) are used in the diagnostics and treatment of cancer because of their nanoscale dimensions of less than 100 nm, excellent stability, biocompatibility, reduced toxicity, and precise targeting capacity. The deep tissue penetration capacity and elevated retention (EPR) effects have further enhanced their applicability in cancer research.7
Different types of NPs, such as organic, inorganic, and hybrid nanoparticles, are used to study cancer biology. Some notable nanoparticles used in cancer diagnostics and therapy are polymeric nanoparticles, dendrimers, liposomes, solid lipid nanoparticles (SLN), nanoemulsion, carbon NPs, quantum dots, metallic NPs, magnetic NPs, and silica NPs. As an example, in vitro experiments associated with mitoxantrone-loaded SLN exhibited enhanced bioavailability, reduced toxicity, and higher efficacy in the elimination of leukemia cells in.8
Nanoformulations can pass through multiple physiological and biological barriers and reach TME, indirectly targeting cancer cells. NPs can cross these barriers and target specific cells due to their small size, surface chemistry, and biocompatibility.
A significant advantage of NPs is their ability to remain stable in the vascular system until they reach TME. They escape the mononuclear phagocyte system and accumulate in the TME through tumor vasculature.9 Furthermore, the physicochemical and functional properties of NPs make them a suitable nanoscale tool for studying cancer biology.
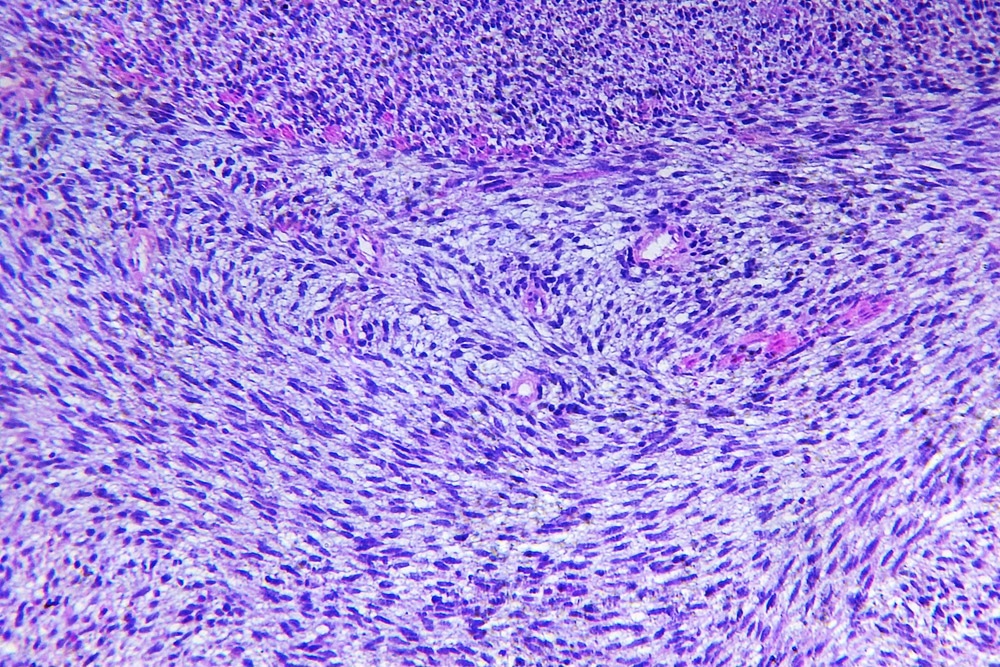
Image Credit: BonD80/Shutterstock.com
Nanoscale Tools to Better Understand Tumor Physiology
NPs have significantly contributed to in vivo imaging, which is a powerful tool in life science research and medical diagnosis using photoacoustic imaging (PAI), ultrasound imaging (USI), and magnetic resonance imaging (MRI). This technique is used for imaging TME, which helps in cancer diagnosis and drug response evaluation.10
Magnetic nanoparticles are used in in vivo imaging with MRI, owing to their large surface area, good biocompatibility, strong magnetic responsiveness, high adsorption capacity, and easy manipulation by external magnetic fields. For tumor imaging, ultramicroscopic paramagnetic iron oxides (USPIOs) and biomolecule-coated small superparamagnetic iron oxide nanoparticles (SPIOs) are used.
The fluorescence imaging technique is also used in physiological and pathological cancer research.11 This technique employs several NPs, including inorganic quantum dots (QDs), for tumor detection. Carbon quantum dots (CQD) possess significant fluorescent properties and are used in cell imaging. The application of fluorescent carbon quantum dots (FCQDs) exhibited a quick accumulation at tumor sites and generated fluorescence images.12
Recent studies have highlighted using microRNAs as biomarkers for cancer diagnosis, therapy, and treatment. MicroRNAs are single-stranded non-coding RNA that regulate genetic expression by inhibiting translation of the target mRNA. These can destabilize mRNA and subsequently inhibit the production of specific proteins. Nanoscale tools are used for the delivery of microRNAs. For instance, microRNA-loaded polycation-hyaluronic acid nanoparticles lead to a downregulation of metastatic cancer load in the lungs.13
Future Directions
Nanotechnology has significantly contributed to the cancer research field, including diagnosis and treatment. Many scientists associated with cancer biology are focussing on improving NP penetration and diffusion to tumor cells. The targeted penetration without affecting other cellular components in the stroma could crucially affect treatment outcome. Stoma cellular components are altered using nanodrugs, which could lead to remodeling of tumor blood vessels or extracellular matrix.
References and Further Reading
- Whiteside, T. L. (2008) The tumor microenvironment and its role in promoting tumor growth. Oncogene, 27(45), pp. 5904–5912. doi.org/10.1038/onc.2008.271
- Cooper, G. M. (2000) The Cell: A Molecular Approach. 2nd edition. Sunderland (MA): Sinauer Associates. The Development and Causes of Cancer. Available from: https://www.ncbi.nlm.nih.gov/books/NBK9963/
- Lugano, R., et al. (2020) Tumor angiogenesis: causes, consequences, challenges and opportunities. Cellular and Molecular Life Sciences, 77(9), pp. 1745-1770. doi.org/10.1007/s00018-019-03351-7
- Gonzalez, H., et al. (2018) Roles of the immune system in cancer: from tumor initiation to metastatic progression. Genes & Development, 32(19-20), pp. 1267-1284. doi.org/10.1101/gad.314617.118
- Dhatchinamoorthy, K., et al. (2021) Cancer Immune Evasion Through Loss of MHC Class I Antigen Presentation. Frontiers in Immunology, 12, p. 636568.
- Malfitano, A. M., et al. (2020) Tumor-Associated Macrophage Status in Cancer Treatment. Cancers (Basel), 12(7), p. 1987.
- Baranwal, J., et al. (2023) Nanoparticles in Cancer Diagnosis and Treatment. Materials (Basel), 16(15), p. 5354. doi.org/10.3390/ma16155354 (Published 2023 Jul 30)
- Gavas, S., et al. (2021) Nanoparticles for Cancer Therapy: Current Progress and Challenges. Nanoscale Research Letters, 16(1), p. 173.
- Ulldemolins, A., et al. (2021) Perspectives of nano-carrier drug delivery systems to overcome cancer drug resistance in the clinics. Cancer Drug Resistance, 4(1), pp. 44-68.
- Yang, Y., et al. (2023) Nanotechnology boosts the efficiency of tumor diagnosis and therapy. Frontiers in Bioengineering and Biotechnology, 11, p. 1249875. doi.org/10.3389/fbioe.2023.1249875
- Etrych, T., et al. (2019) Fluorescence Imaging as a Tool in Preclinical Evaluation of Polymer-Based Nano-DDS Systems Intended for Cancer Treatment. Pharmaceutics, 11(9), p. 471.
- Latha, B. D., et al. (2023) Fluorescent carbon quantum dots for effective tumor diagnosis: A comprehensive review. Biomedical Engineering Advances, 5, p. 100072. doi.org/10.1016/j.bea.2023.100072
- Wu, S. G., et al. (2019). MicroRNA in Lung Cancer Metastasis. Cancers (Basel), 11(2), p. 265.
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.