In an innovative study, scientists at Mudanjiang Medical University improved a poly (L-lactic acid) (PLLA) nanofibrous membrane with silver nanoparticles (AgNPs) and curcumin to promote the healing of diabetic wounds. This sophisticated dressing addresses vital obstacles that impede diabetic patients' recuperation, including oxidative stress, bacterial infections, and inflammation. The study's findings point to a potential treatment plan that could completely change the way wounds caused by diabetes are treated. The study has been published in Burns & Trauma.
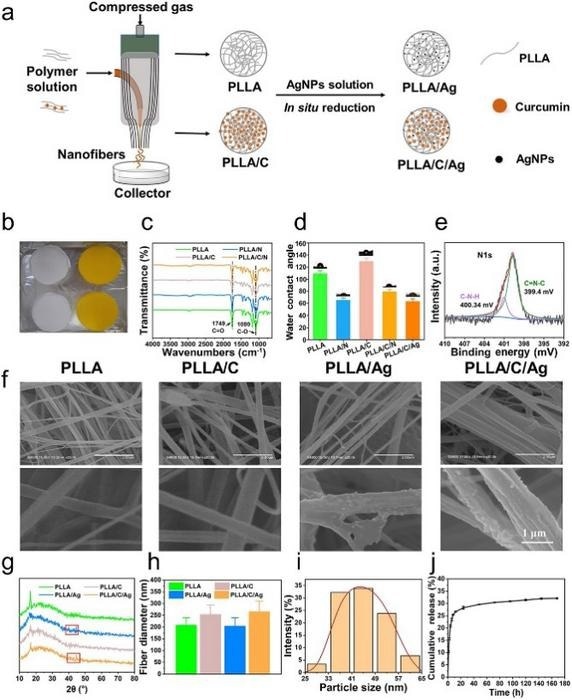
Development and physicochemical properties of PLLA nanofibrous membranes. Image Credit: Burns & Trauma
Diabetes-related wounds are infamously difficult to heal because of their protracted inflammation and increased risk of infection. Conventional therapies typically do not dynamically engage with the wound environment; instead, they primarily provide passive protection. The development of bioactive dressings, such as curcumin (PLLA/C/Ag) membranes and poly (L-lactic acid) (PLLA) nanofibrous membranes infused with AgNPs, represents a significant move toward treatments that actively address imbalances in the wound healing process and provide a more successful approach to the management of diabetic wounds.
The researchers are associated with the Mudanjiang Medical University and affiliated institutions. These membranes, which are infused with curcumin and silver nanoparticles, aim to significantly improve the healing processes of diabetic wounds by addressing underlying problems such as excessive inflammation and infection.
The goal of this research was to create PLLA/C/Ag nanofibrous membranes by air-jet spinning, which would allow for the consistent fiber distribution needed for efficient therapeutic delivery. The membranes have two advantages: strong antibacterial activity that lowers the risk of infection and antioxidant qualities that lessen damaging reactive oxygen species in wound environments. The ability of the membranes to stimulate angiogenesis and collagen deposition—two essential healing processes—was shown in vivo tests on diabetic mice.

Image Credit: megaflopp/Shutterstock.com
These results demonstrate that PLLA/C/Ag membranes are a significant therapeutic innovation for diabetic wound management, with the potential for broader chronic wound care applications. They not only protect wounds but also actively support and accelerate the healing process.
The PLLA/C/Ag membranes are a significant breakthrough in diabetic wound care. Their ability to effectively modulate the wound environment and enhance healing could establish a new standard in treatment, providing hope to millions affected by diabetes-related complications.
Dr. Yanhui Chu, Study Principal Investigator, Mudanjiang Medical University
The application of PLLA/C/Ag nanofibrous membranes in clinical settings has the potential to revolutionize the management of diabetic wounds by providing a more proactive and efficient strategy. This technology could be widely used in treating a variety of chronic wounds in addition to managing diabetes, opening the door for further advancements in bioactive wound dressings. In addition to advancing the knowledge of wound care, this work opens up new avenues for the creation of adaptable wound care solutions.
Journal Reference:
Wu, Y., et al. (2024) Immunomodulatory poly(L-lactic acid) nanofibrous membranes promote diabetic wound healing by inhibiting inflammation, oxidation and bacterial infection. Burns & Trauma. doi.org/10.1093/burnst/tkae009