Reviewed by Alex SmithSep 20 2021
Researchers from Hokkaido University and their collaborators in Japan have identified a strategy to help certain patients overcome resistance to immunotherapy treatment for cancer. The approach has been proven in mice experiments and was described in the Journal for ImmunoTherapy of Cancer.
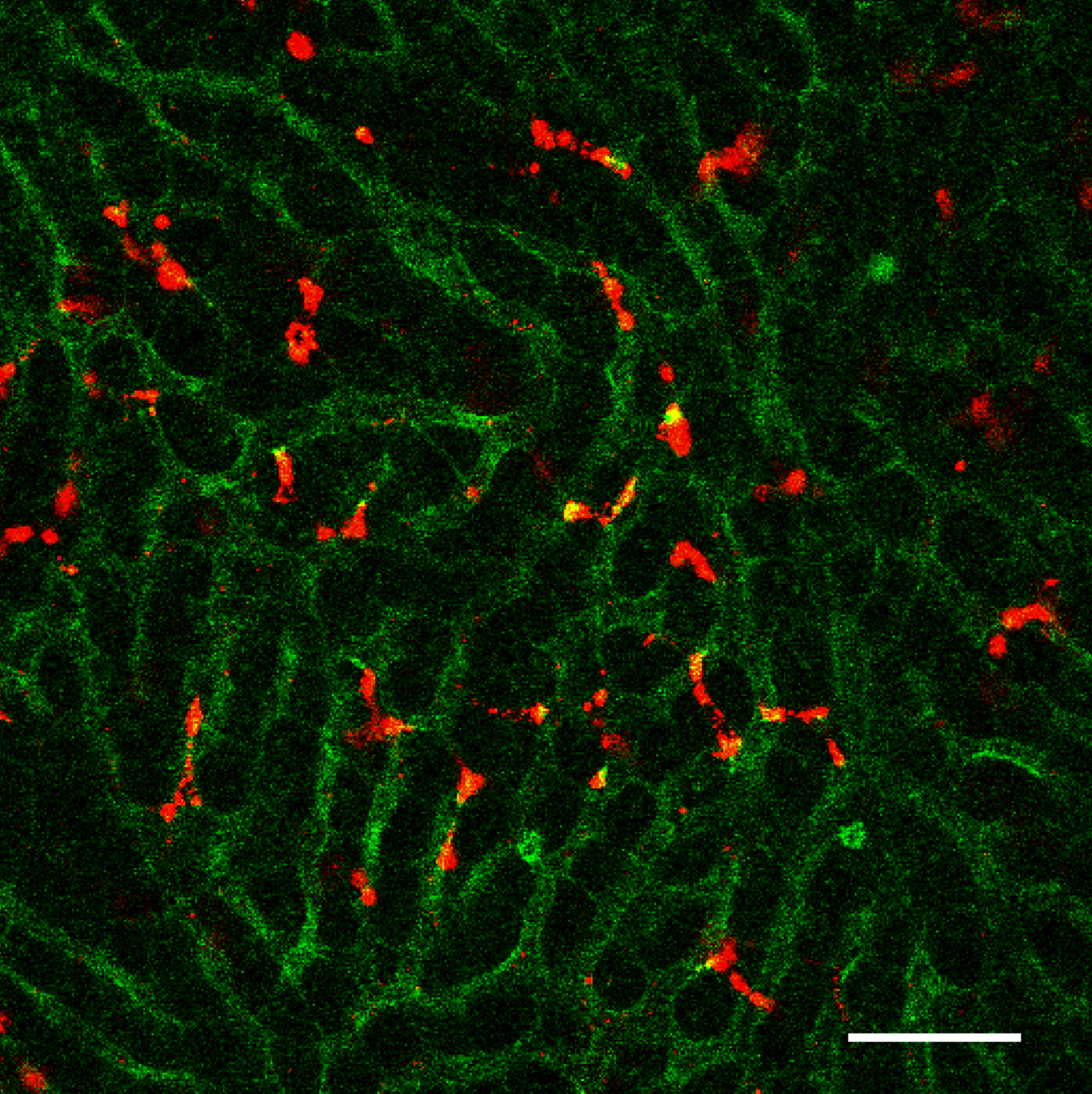 After intravenous injection into mice, STING-lipid nanoparticles (red) transported through blood vessels(green) accumulate in the liver. Image Credit: Takashi Nakamura, et al. Journal for ImmunoTherapy of Cancer. July 2nd, 2021.
After intravenous injection into mice, STING-lipid nanoparticles (red) transported through blood vessels(green) accumulate in the liver. Image Credit: Takashi Nakamura, et al. Journal for ImmunoTherapy of Cancer. July 2nd, 2021.
The checkpoint protein activation on the immune cell surface helps control the immune response by inhibiting the proteins from arbitrarily attacking the body’s other cells. However, certain cancer cells can hijack this mechanism, inhibiting an immune response against them. Recently, researchers developed immune checkpoint inhibitors with the ability to counteract this approach; however, some patients are resistant to the treatments.
Researchers at Hokkaido University and the Aichi Institute of Technology have now found a new approach to overcome this problem. They developed an exclusively designed lipid nanoparticle with the ability to carry immunity-activating molecules into immune cells in the liver known as macrophages.
Named YSK12-C4, the lipid has a high affinity for immune cells. Upon intravenously injecting the lipid into mice with metastatic melanoma, it could deliver signaling molecules, named cyclic dinucleotides, across the cell membranes of their liver macrophages, where they activated the production of immune-associated proteins known as type 1 interferons through a stimulator of an interferon gene (STING) pathway.
These were released into the blood, stimulating another kind of immune cell known as natural killer cells in the spleen and lung, which generated interferon-gamma within the lung metastases.
This treatment itself only led to a mild anti-tumor effect. The reason is that the type 1 interferons and interferon-gamma stimulated the expression of a protein named PD-L1 on the cancer cells. PD-L1 inhibits a powerful tumor-killing immune reaction of natural killer cells that express PD-1.
However, when an anti-PD-1 immunotherapy treatment was administered, the cancer cells were inhibited from turning off the natural killer cells, which in turn became armed and able to initiate a full-scale attack.
The findings suggest that our lipid nanoparticles carrying immune-signaling molecules convert the immune status from immunologically cold to immunologically hot. This could lead to the development of a promising adjuvant that reduces resistance to anti-PD-1 antibody treatment in some cancer patients.
Takashi Nakamura, Faculty of Pharmaceutical Sciences, Hokkaido University
Additional studies will have to analyze whether the treatment can lead to liver toxicity and whether other signaling molecules can be used.
This study was supported by the Japanese Government (MEXT), Platform Project for Supporting in Drug Discovery and Life Science Research (Platform for Drug Discovery, Informatics, and Structural Life Science) from the Japan Agency for Medical Research and Development (AMED) and Hokkaido University, Global Facility Center (GFC), Pharma Science Open Unit (PSOU), financially supported by MEXT under “Support Program for Implementation of New Equipment Sharing System.”
Journal Reference:
Nakamura, T., et al. (2021) STING agonist loaded lipid nanoparticles overcome anti-PD-1 resistance in melanoma lung metastasis via NK cell activation. Journal for ImmunoTherapy of Cancer. doi.org/10.1136/jitc-2021-002852.