Nov 14 2008
Medical researchers are looking at any number of new methods to get drugs to specific locations in the body. Some methods are efficient but less safe, while others are safe but often fail to deliver. Now a nontoxic nanoparticle developed by researchers at Penn State University is proving to be an all-around effective delivery system for both therapeutic drugs and the fluorescent dyes that can track their delivery. In an article appearing in an upcoming print issue of Nano Letters (currently available online), an interdisciplinary group of materials scientists, chemists, bioengineers, physicists, and pharmacologists show that calcium phosphate particles ranging in size from 20 to 50 nanometers will successfully enter cells and dissolve harmlessly, releasing their cargo of drugs or dye.
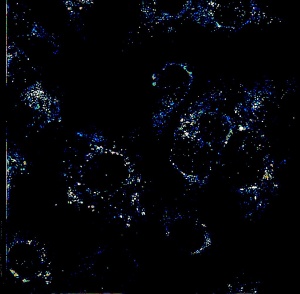 Bovine aortic endothelial cells are treated with a drug that does not permit acidity to increase enough to dissolve the nanoparticles. Dark circles are the cell nuclei. Image is approx. 1/10 millimeter across. Image: Hari S. Muddana
Bovine aortic endothelial cells are treated with a drug that does not permit acidity to increase enough to dissolve the nanoparticles. Dark circles are the cell nuclei. Image is approx. 1/10 millimeter across. Image: Hari S. Muddana
Measuring the activity of particles this size requires specialized techniques. Peter Butler, associate professor of bioengineering, and his students used high speed lasers to measure the size of fluorescent dye-containing particles from their diffusion in solution. “We use a technique called time correlated single photon counting,” Butler says. “This uses pulses of laser light to read the time, on the order of nanoseconds, that molecules fluoresce.” With this method his group was able to measure the size of the particles and their dispersion in solution, in this case a phosphate-buffered saline that is used as a simple model for blood.
“What we did in this study was to change the original neutral pH of the solution, which is similar to blood, to a more acidic environment, such as around solid tumors and in the parts of the cell that collect the nanoparticles-containing fluid immediately outside the cell membrane and bring it into the cell. When we lower the pH, the acidic environment dissolves the calcium phosphate particle. We can see that the size of the particles gets very small, essentially down to the size of the free dye that was inside the particles. That gives us evidence that this pH change can be used as a mechanism to release any drug that is encapsulated in the particle,” Butler explains.
Although the primary use envisioned for these particles is for targeted cancer therapy, Butler’s group is interested in their ability to deliver various drugs that have been shown to inhibit cell growth associated with vascular disease. Several drugs have been shown in cultures to be promising for reducing atherosclerosis (hardening of the arteries) and restenosis (the narrowing of blood vessels after balloon angioplasty). The problem has been in delivering any of these drugs to a target, Butler says.
Ceramide, a chemotherapeutic molecule that initiates cell death in cancer cells, has the ability to slow growth in healthy cells. Mark Kester, professor of pharmacology, and associate professor of pharmacology Jong Yun have optimized ceramide for both cancer and vascular disease. In an experiment performed by Kester’s and Yun’s groups in the Penn State Milton S. Hershey Medical Center and Penn State College of Medicine using human vascular smooth muscle cells in vitro, ceramide encapsulated in calcium phosphate nanoparticles reduced growth of muscle cells by up to 80 percent at a dose 25 times lower than ceramide administered freely, without damaging the cells.
The calcium phosphate nanoparticles were developed by Jim Adair, professor of materials science and engineering, and his students. The nanoparticles have several benefits other drug delivery systems do not, according to lead author Thomas Morgan, one of the graduate students in Adair’s group. Unlike quantum dots, which are composed of toxic metals, calcium phosphate is a safe, naturally occurring mineral that already is present in substantial amounts in the bloodstream. “What distinguishes our method are smaller particles (for uptake into cells), no agglomeration (particles are dispersed evenly in solution), and that we put drugs or dyes inside the particle where they are protected, rather than on the surface. For reasons we don’t yet understand, fluorescent dyes encapsulated within our nanoparticles are four times brighter than free dyes,” Morgan says.
“Drugs and dyes are expensive,” he continues, “but an advantage of encapsulation is that you need much less of them. We can make high concentrations in the lab, and dilute them way down and still be effective. We even believe we can combine drug and dye delivery for simultaneous tracking and treatment. That’s one of the things we are currently working on.”
Contributors to the article in Nano Letters were graduate students Thomas Morgan, chemistry, Erhan Altinoglu and Amra Tabakovic, materials science and engineering, and former group member, Sara Rouse, Ph.D. in materials; graduate students Hari Muddana and Tristan Tabouillot, bioengineering; graduate student Timothy Russin, physics; graduate student Sriram Shanmugavelandy, pharmacology; Peter Butler, associate professor of bioengineering; Peter Eklund, distinguished professor of physics and materials science and engineering; Jong Yun, associate professor of pharmacology; Mark Kester, professor of pharmacology; and Jim Adair, professor of materials science and engineering. Support was provided by multiple agencies, including NSF, NASA, Keystone Nano, Inc. and by grants to Peter Butler from the National Heart, Lung, and Blood Institute and the National Science Foundation.
The Penn State Materials Research Institute provides facilities and technical staff to support the research of more than 200 faculty groups involved in materials research at Penn State. www.mri.psu.edu