A team led by scientists from The Scripps Research Institute (TSRI) and the International AIDS Vaccine Initiative (IAVI) has unveiled a new technique for vaccine design that could be particularly useful against HIV and other fast-changing viruses.
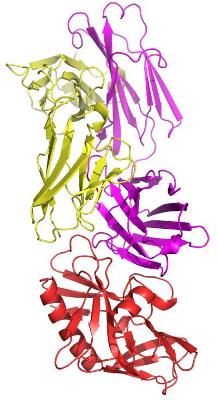 The researchers demonstrated their new technique by engineering a compound that has promise to initiate an otherwise rare immune response against many types of HIV. Here, the germline-targeting immunogen eOD-GT6 (red) is shown bound to its target, the germline VRC01 antibody (magenta and yellow). Credit: Photo courtesy of The Scripps Research Institute.
The researchers demonstrated their new technique by engineering a compound that has promise to initiate an otherwise rare immune response against many types of HIV. Here, the germline-targeting immunogen eOD-GT6 (red) is shown bound to its target, the germline VRC01 antibody (magenta and yellow). Credit: Photo courtesy of The Scripps Research Institute.
The report, which appears March 28, 2013, in Science Express, the early online edition of the journal Science, offers a step toward solving what has been one of the central problems of modern vaccine design: how to stimulate the immune system to produce the right kind of antibody response to protect against a wide range of viral strains. The researchers demonstrated their new technique by engineering an immunogen (substance that induces immunity) that has promise to reliably initiate an otherwise rare response effective against many types of HIV.
"We're hoping to test this immunogen soon in mice engineered to produce human antibodies, and eventually in humans," said team leader William R. Schief, who is an associate professor of immunology and member of the IAVI Neutralizing Antibody Center at TSRI.
Seeking a Better Way
For highly variable viruses such as HIV and influenza, vaccine researchers want to elicit antibodies that protect against most or all viral strains—not just a few strains, as seasonal flu vaccines currently on the market. Vaccine researchers have identified several of these broadly neutralizing antibodies from long-term HIV-positive survivors, harvesting antibody-producing B cells from blood samples and then sifting through them to identify those that produce antibodies capable of neutralizing multiple strains of HIV. Such broadly neutralizing antibodies typically work by blocking crucial functional sites on a virus that are conserved among different strains despite high mutation elsewhere.
However, even with these powerful broadly neutralizing antibodies in hand, scientists need to find a way to elicit their production in the body through a vaccine. "For example, to elicit broadly neutralizing antibodies called VRC01-class antibodies that neutralize 90 percent of known HIV strains, you could try using the HIV envelope protein as your immunogen," said Schief, "but you run into the problem that the envelope protein doesn't bind with any detectable affinity to the B cells needed to launch a broadly neutralizing antibody response."
To reliably initiate that VRC01-class antibody response, Schief and his colleagues therefore sought to develop a new method for designing vaccine immunogens.
From Weak to Strong
Joseph Jardine, a TSRI graduate student in the Schief laboratory, evaluated the genes of VRC01-producing B cells in order to deduce the identities of the less mature B cells—known as germline B cells—from which they originate. Germline B cells are major targets of modern viral vaccines, because it is the initial stimulation of these B cells and their antibodies that leads to a long-term antibody response.
In response to vaccination, germline B cells could, in principle, mature into the desired VRC01-producing B cells—but natural HIV proteins fail to bind or stimulate these germline B cells so they cannot get the process started. The team thus set out to design an artificial immunogen that would be successful at achieving this.
Jardine used a protein modeling software suite called Rosetta to improve the binding of VRC01 germline B cell antibodies to HIV's envelope protein. "We asked Rosetta to look for mutations on the side of the HIV envelope protein that would help it bind tightly to our germline antibodies," he said.
Rosetta identified dozens of mutations that could help improve binding to germline antibodies. Jardine then generated libraries that contained all possible combinations of beneficial mutations, resulting in millions of mutants, and screened them using techniques called yeast surface display and FACS. This combination of computational prediction and directed evolution successfully produced a few mutant envelope proteins with high affinity for germline VRC01-class antibodies.
Jardine then focused on making a minimal immunogen—much smaller than HIV envelope—and so continued development using the "engineered outer domain (eOD)" previously developed by Po-Ssu Huang in the Schief lab while Schief was at the University of Washington. Several iterative rounds of design and selection using a panel of germline antibodies produced a final, optimized immunogen—a construct they called eOD-GT6.
A Closer Look
To get a better look at eOD-GT6 and its interaction with germline antibodies, the team turned to the laboratory of Ian A. Wilson, chair of the Department of Integrative Structural and Computational Biology and a member of the IAVI Neutralizing Antibody Center at TSRI.
Jean-Philippe Julien, a senior research associate in the Wilson laboratory, determined the 3D atomic structure of the designed immunogen using X-ray crystallography—and, in an unusual feat, also determined the crystal structure of a germline VRC01 antibody, plus the structure of the immunogen and antibody bound together.
"We wanted to know whether eOD-GT6 looked the way we anticipated and whether it bound to the antibody in the way that we predicted—and in both cases the answer was 'yes'," said Julien. "We also were able to identify the key mutations that conferred its reactivity with germline VRC01 antibodies."
Mimicking a Virus
Vaccine researchers know that such an immunogen typically does better at stimulating an antibody response when it is presented not as a single copy but in a closely spaced cluster of multiple copies, and with only its antibody-binding end exposed. "We wanted it to look like a virus," said Sergey Menis, a visiting graduate student in the Schief laboratory.
Menis therefore devised a tiny virus-mimicking particle made from 60 copies of an obscure bacterial enzyme and coated it with 60 copies of eOD-GT6. The particle worked well at activating VRC01 germline B cells and even mature B cells in the lab dish, whereas single-copy eOD-GT6 did not.
"Essentially it's a self-assembling nanoparticle that presents the immunogen in a properly oriented way," Menis said. "We're hoping that this approach can be used not just for an HIV vaccine but for many other vaccines, too."
The next step for the eOD-GT6 immunogen project, said Schief, is to test its ability to stimulate an antibody response in lab animals that are themselves engineered to produce human germline antibodies. The difficulty with testing immunogens that target human germline antibodies is that animals typically used for vaccine testing cannot make those same antibodies. So the team is collaborating with other researchers who are engineering mice to produce human germline antibodies. After that, he hopes to learn how to drive the response, from the activation of the germline B cells all the way to the production of mature, broadly neutralizing VRC01-class antibodies, using a series of designed immunogens.
Schief also hopes they will be able to test their germline-targeting approach in humans sooner rather than later, noting "it will be really important to find out if this works in a human being."