Oct 8 2014
Scientists have been laboring to detect cancer and a host of other diseases in people using promising new biomarkers called "exosomes." Indeed, Popular Science magazine named exosome-based cancer diagnostics one of the 20 breakthroughs that will shape the world this year. Exosomes could lead to less invasive, earlier detection of cancer, and sharply boost patients' odds of survival.
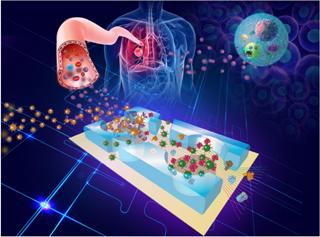 The prototype lab-on-a-chip is made of a widely used silicone rubber called polydimethylsiloxane and uses a technique called 'on-chip immunoisolation.' Credit: University of Kansas/KU News Service
The prototype lab-on-a-chip is made of a widely used silicone rubber called polydimethylsiloxane and uses a technique called 'on-chip immunoisolation.' Credit: University of Kansas/KU News Service
"Exosomes are minuscule membrane vesicles — or sacs — released from most, if not all, cell types, including cancer cells," said Yong Zeng, assistant professor of chemistry at the University of Kansas. "First described in the mid-'80s, they were once thought to be 'cell dust,' or trash bags containing unwanted cellular contents. However, in the past decade scientists realized that exosomes play important roles in many biological functions through capsuling and delivering molecular messages in the form of nucleic acids and proteins from the donor cells to affect the functions of nearby or distant cells. In other words, this forms a crucial pathway in which cells talk to others."
While the average piece of paper is about 100,000 nanometers thick, exosomes run just 30 to 150 nanometers in size. Because of this, exosomes are hard to separate out and test, requiring multiple-step ultracentrifugation — a tedious and inefficient process requires long stretches in the lab, according to scientists.
"There aren't many technologies out there that are suitable for efficient isolation and sensitive molecular profiling of exosomes," said Zeng. "First, current exosome isolation protocols are time-consuming and difficult to standardize. Second, conventional downstream analyses on collected exosomes are slow and require large samples, which is a key setback in clinical development of exosomal biomarkers."
Now, Zeng and colleagues from the University of Kansas Medical Center and KU Cancer Center have just published a breakthrough paper in the Royal Society of Chemistry journal describing their invention of a miniaturized biomedical testing device for exosomes. Dubbed the "lab-on-a-chip," the device promises faster result times, reduced costs, minimal sample demands and better sensitivity of analysis when compared to the conventional bench-top instruments now used to examine the tiny biomarkers.
"A lab-on-a-chip shrinks the pipettes, test tubes and analysis instruments of a modern chemistry lab onto a microchip-sized wafer," Zeng said. "Also referred to as 'microfluidics' technology, it was inspired by revolutionary semiconductor electronics and has been under intensive development since the 1990s. Essentially, it allows precise manipulation of minuscule fluid volumes down to one trillionth of a liter or less to carry out multiple laboratory functions, such as sample purification, running of chemical and biological reactions, and analytical measurement."
Zeng and his fellow researchers have developed the lab-on-a-chip for early detection of lung cancer — the number-one cancer killer in the U.S. Today, lung cancer is detected mostly with an invasive biopsy, after tumors are larger than 3 centimeters in diameter and even metastatic, according to the KU researcher.
Using the lab-on-a-chip, lung cancer could be detected much earlier, using only a small drop of a patient's blood.
"Most lung cancers are first diagnosed based on symptoms, which indicate that the normal lung functions have been already damaged," Zeng said. "Unlike some cancer types such as breast or colon cancer, no widely accepted screening tool has been available for detecting early-stage lung cancers. Diagnosis of lung cancer requires removing a piece of tissue from the lung for molecular examination. Tumor biopsy is often impossible for early cancer diagnosis as the developing tumor is too small to see by the current imaging tools. In contrast, our blood-based test is minimally invasive, inexpensive, and more sensitive, thus suitable for large population screening to detect early-stage tumors."
Zeng said the prototype lab-on-a-chip is made of a widely used silicone rubber called polydimethylsiloxane and uses a technique called "on-chip immunoisolation."
"We used magnetic beads of 3 micrometers in diameter to pull down the exosomes in plasma samples," Zeng said. "In order to avoid other interfering species present in plasma, the bead surface was chemically modified with an antibody that recognizes and binds with a specific target protein — for example, a protein receptor — present on the exosome membrane. The plasma containing magnetic beads then flows through the microchannels on the diagnostic chip in which the beads can be readily collected using a magnet to extract circulating exosomes from the plasma."
Beyond lung cancer, Zeng said the lab-on-a-chip could be used to detect a range of potentially deadly forms of cancer.
"Our technique provides a general platform to detecting tumor-derived exosomes for cancer diagnosis," he said. "In addition to lung cancer, we've also tested for ovarian cancer in this work. In theory, it should be applicable to other types of cancer. Our long-term goal is to translate this technology into clinical investigation of the pathological implication of exosomes in tumor development. Such knowledge would help develop better predictive biomarkers and more efficient targeted therapy to improve the clinical outcome."