Sep 6 2017
A major amount of secondary nerve damage after a spinal cord injury is due to inflammation and internal scarring that hinders the ability of the nervous system to repair itself.
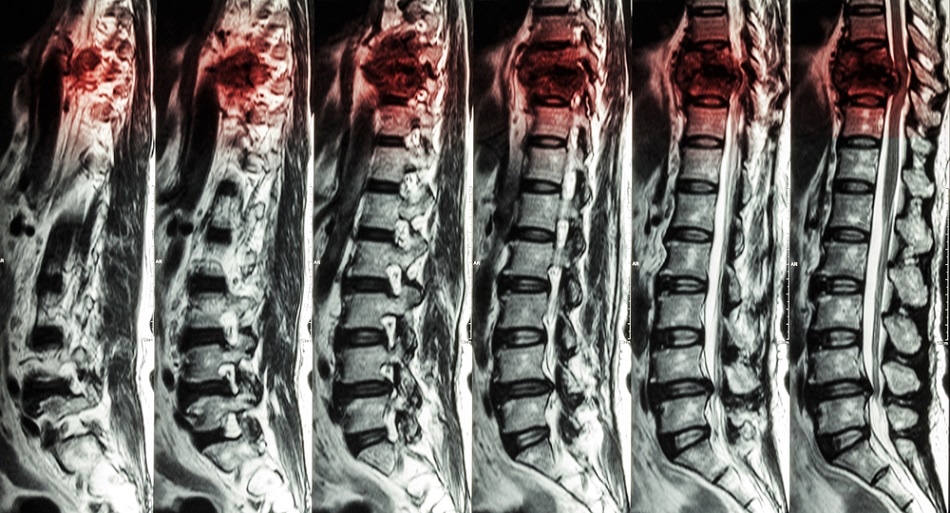 Puwadol Jaturawutthichai/ Shutterstock.com
Puwadol Jaturawutthichai/ Shutterstock.com
A recent Northwestern Medicine study states that a biodegradable nanoparticle injected after a spinal cord trauma prevented the inflammation and internal scarring that hinders the repair process.
Consequently, when mice with a spinal cord injury were given the nanoparticle injection, they were able to walk better than those that were not given.
The treatment could potentially prevent secondary damage to the spinal cord in humans after an injury, if given a few hours after the accident by Paramedics in an ambulance or in an emergency room.
It’s not a cure. There is still the original damage, but we were able to prevent the secondary damage. It’s an exciting potential treatment. We really believe this is something we’ll be able to take to the clinic.
Dr. Jack Kessler, Co-senior Author and a Professor of Neurology, Feinberg School of Medicine, Northwestern University
Additional studies would need to ratify the safety of the injected nanoparticle, Kessler said, but he observed Scientists have not seen any indications of toxicity thus far.
The details of the study were published in the August 24th issue of Neurobiology of Disease.
The nanoparticles function by attaching to the cells that cause the inflammation — inflammatory monocytes — and diverting them to the spleen. The particles are composed of poly(lactic-co-glycolic) acid, a biocompatible substance already approved by the Food and Drug Administration (FDA) for application in re-absorbable sutures.
These particles were created in the lab of Northwestern Scientist Stephen Miller, and they are also are FDA approved as an investigational drug for a new clinical trial in celiac disease.
The study results suggest nanoparticle infusion could offer a novel and practical potential treatment for human spinal cord injury, a condition for which there are currently no effective treatments.
Stephen Miller, the Judy Gugenheim Research Professor of Microbiology-Immunology, Feinberg School of Medicine, Northwestern University
After a spinal cord injury, blood cells that usually could not enter the nervous system break through the protective blood brain barrier and flood the injury site. They discharge noxious chemicals, called inflammatory cytokines, which call in extra inflammatory blood cells. These cells damage the central nervous system tissue more by causing neuronal cell death and scar formation that prevents recovery from paralysis.
Two types of neurons die. Myelin is one type that surrounds the nerve fibers and allows them to convey signals through the nervous system. If the myelin sheath is lost, the cells cannot conduct signals. Axons, the other cells that die, are the long fibers extending from the neurons that convey signals from neuron to neuron.
“The new treatment is unusual because it is potentially immediately translatable to human beings,” Kessler said. “All we have to do is literally inject these beads into the blood stream. It doesn’t require surgery or any fancy intervention.”
The miniature beads also are highly stable and can be stored in a syringe, Kessler noted. “An emergency medical technician at the site of an accident or somebody in an emergency room when someone is brought in can give this injection immediately,” he said.
Other Researchers have tried methods to stop inflammatory monocytes from getting into the nervous system after a spinal cord injury, but those approaches blocked both advantageous and harmful cells. The helpful cells actually clean up the damage from the trauma and restrict the scarring, so earlier efforts resulted in just a modest improvement in cell death, scarring, and repair.
The nanoparticle technology is commercially developed by Cour Pharmaceuticals Development Co., which is partnering with Miller to provide this new method to patients. Miller is a Co-founder of Cour and a Member of the Scientific Advisory Board.
Miller also is a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University.
Northwestern coauthors include Su Ji Jeong, John G. Cooper, Igal Ifergan, Tammy L. McGuire, Dan Xu, Zoe Hunter, Sripadh Sharma and Derrick McCarthy.
This study was supported by grants EB013198 from the National Institute of Biomedical Imaging and Bioengineering and NS026543 and F30NS093811 from National Institute of Neurological Disorders and Stroke, all of the National Institutes of Health.