Jun 15 2021
The rare lung disease is so complicated that its acronym is difficult to pronounce. However, for infants who were unfortunate enough to be born with this disorder, the outcome is generally fatal.
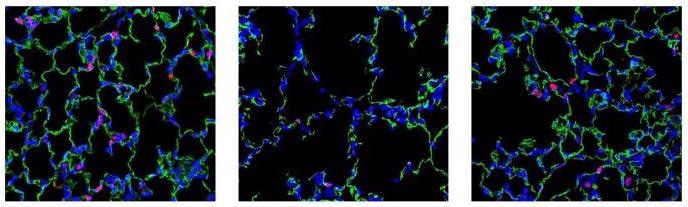 Left: normal mouse lung tissue showing a healthy density of blood vessels. Middle: example of abnormal, diseased tissue with reduced STAT3 activation. Right: tissue from a treated mouse. Green depicts blood vessels; Red shows activated STAT3. Image Credit: Cincinnati Children's.
Left: normal mouse lung tissue showing a healthy density of blood vessels. Middle: example of abnormal, diseased tissue with reduced STAT3 activation. Right: tissue from a treated mouse. Green depicts blood vessels; Red shows activated STAT3. Image Credit: Cincinnati Children's.
The disease is known as alveolar capillary dysplasia with misalignment of the pulmonary veins, or ACDMPV for short. According to a study, the disease is associated with mutations in the FOXF1 gene. Medical experts throughout the world have recorded around 200 cases, but an unestimated number of infants could have died without the disorder ever being diagnosed, stated the National Organization for Rare Disorders.
The disease is induced by genetic changes that inhibit the formation of proper blood vessels in the lungs. Within a few days or weeks post birth, infants turn blue because of the absence of oxygen while blood pressure increases inside their lungs. The few infants who get to live do so by receiving exceptionally rare infant-sized lung transplants.
Now, a new study headed by experts from Cincinnati Children’s and the University of Cincinnati has reported about helping mice (with a FOXF1 mutation that is identical to human ACDMPV patients) live longer with this fatal disease. This was done by applying high-tech nanoparticles to send a STAT3 gene into the lungs to trigger the growth of blood vessels.
STAT3 is a crucial downstream target of the FOXF1 gene and its delivery can rectify the vascular deficiency in ACDMPV mice. The study results were published online in the Circulation journal on June 11th, 2021.
If these findings can be matched in human analyses in the future, this success can potentially boost the speed of development for other nanoparticle-based treatments for many medical conditions, stated the study co-authors.
Nanoparticle carriers have shown minimal toxicity and have accelerated the development of novel therapies for human cancers, diabetes, and chronic inflammatory disorders. We have developed a unique nanoparticle delivery system that can deliver genes capable of stimulating micro-vessel growth in the newborn lung.
Vlad Kalinichenko, MD, PhD, Study Senior Author and Member of the Center for Lung Regenerative Medicine and Perinatal Institute, Cincinnati Children’s Hospital Medical Center
Kalinichenko added, “This study shows that a single injection of the nanoparticles with the STAT3 gene vector was sufficient to increase alveolar-capillary density, prevent excessively high blood pressures and dramatically improve survival.”
Around 70% of mice born with ACDMPV die in less than 28 days of birth without treatment. The new therapy reduced this mortality rate to 35%, stated Fei Sun, PhD, the first author of the study and a member of the Center for Lung Regenerative Medicine at Cincinnati Children’s.
Gene-Driven Therapy but not Gene Editing
This nanoparticle method is different from gene replacement therapies that can cause permanent changes in the body. It involves materials that do not remain in the body for more than seven days. Yet, in the mice examined so far, a single therapy early after the birth was sufficient to divert a whole stream of later-developing issues that take place with ACDMPV.
The treatment works by sending an engineered nanoparticle composed of many fatty acids, polymers and a small amount of cholesterol that transports the non-integrating STAT3 gene, which consequently encourages the growth of blood vessels in the lung tissue.
Kalinichenko and collaborators also noted the molecular processes involved as part of their ongoing analyses of lung development. The nanoparticle was designed with support from Zicheng Deng and Andrew Dunn, who are both graduate students mentored by Donglu Shi, PhD, from the Materials Science and Engineering Program at the University of Cincinnati.
With the presence of more blood vessels, the rapidly growing lungs in the newborns developed in a closer-to-normal fashion, without triggering harmful molecular “remodeling” signals that can lead to permanent malformations and even death from lung failure.
The study explains how the therapy enhanced various measures of heart, lung and blood vessel health, such as the ratio of pulmonary acceleration time to pulmonary ejection time (PAT/PET), blood pressure in the right ventricle, arterial oxygenation levels, the diameter of pulmonary arteries and also the thickness of their walls.
Next Steps
More studies need to be completed before nanoparticles can be tested in human newborns with ACDMPV, such as safety tests and establishing whether recurrent treatments would be required.
Journal Reference:
Sun, F., et al. (2021) Nanoparticle Delivery of STAT3 Alleviates Pulmonary Hypertension in a Mouse Model of Alveolar Capillary Dysplasia. Circulation. doi.org/10.1161/CIRCULATIONAHA.121.053980.