Scientists at Tufts University School of Engineering are aiming to gain a reputation for precision targeting in the area of drug delivery.
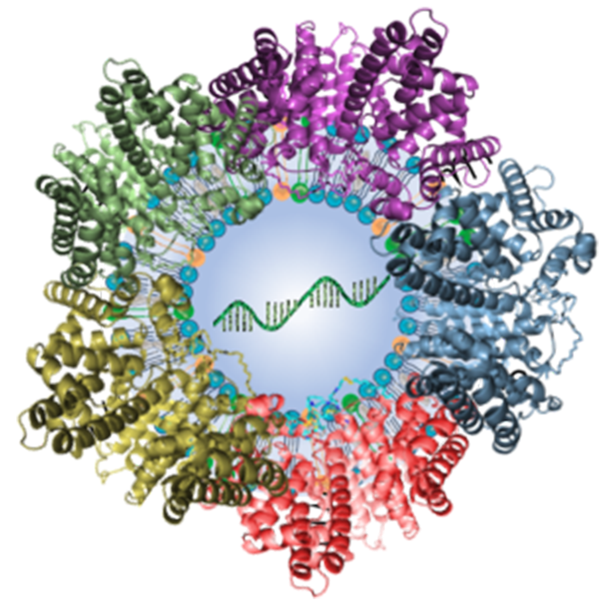 Illustration of lipid nanoparticle packed with mRNA and surrounded by attached plasma proteins. Image Credit: Qiaobing Xu, Tufts University.
Illustration of lipid nanoparticle packed with mRNA and surrounded by attached plasma proteins. Image Credit: Qiaobing Xu, Tufts University.
Their tools: minute lipid-based nanoparticles (LNPs) that can be tweaked to adhere to specific organs, tissues, even cell types within the body. Their most recent creation: LNPs that transport genetic instructions straight into the lungs.
Even before LNP delivery had its first major debut with COVID-19 vaccines, Xu and his team have been developing the technology that will be relevant to a much wider range of diseases by targeting treatments to precise tissues and organs, which helps lessen harmful effects on other, healthy areas of the body.
In a study published in the Proceedings of the National Academy of Sciences, a team headed by Tufts scientist Qiaobing Xu, along with collaborators at Harvard Medical School and the University of Massachusetts, Boston, filled the LNPs with mRNA — the same genetic material added in COVID-19 vaccines, but this time coding for a regular gene, Tsc2, that is mutated in individuals with a rare disease known as lymphangioleiomyomatosis (LAM).
The mutated Tsc2 makes smooth muscle tissue grow excessively, forming cysts that resemble large gaps or holes in the lungs on a CT scan or an X-Ray. In a mouse model of LAM, delivering a regular Tsc2 gene straight to the lungs led to a substantial reduction in cysts.
The effect was quite impressive. The mRNA-packed LNPs could be a promising intervention for this awful disease, and we hope to carry it further into clinical trials.
Qiaobing Xu, Study Corresponding Author and Professor of Biomedical Engineering, Tufts University
The extraordinary achievement follows on from previous innovative research, where Xu and his team developed LNPs that transport gene-editing packages into cells of the immune system or the liver or even across the blood-brain barrier to targeted areas of the brain.
The present study does not include gene editing, which splices out a bad gene and swaps it with a good one. Here, it is similar to overwriting the bad gene that is still present with a temporary code (the mRNA) that disappears over time, necessitating repeat doses. Would it be conceivable to try a more permanent gene-editing method to LAM?
We were able to demonstrate that we could deliver gene editing to the lungs, but it showed up in the liver as well. The size and components of the gene-editing kit may have effected the LNPs’ ability to selectively target the lungs in this case. Delivering the smaller mRNA package is a lot more selective.
Min Qiu, Study Co-First Author and Principal Investigator, Fudan University
Min Qiu, the co-first author of the study, was a former postdoctoral researcher in the Xu group at Tufts.
The team is presently involved in tweaking the LNPs to allow more targeted gene editing to the lungs. One may wonder how they can target the LNPs to the lungs. The LNPs are fundamentally miniature bubbles of fat (lipid) and other molecules. Similar to the mRNA, the LNPs were also used in two of the key vaccines approved for guarding against COVID-19.
The twist incorporated by the Tufts scientists to make the LNPs target a particular organ like the lungs comes from how they alter the lipids and other molecules making up the minute bubbles. The bubbles are produced with a bilayer of lipids which enfold the contents.
Every lipid can be illustrated as possessing chemical parts — a head that points towards a watery environment — either to the outside, or the inside of the bubble where the mRNA or gene-editing system is packed; a tail that indicates to the middle of the bilayer, and a linker between the two. Altering any of those parts can alter where the LNPs might reach in the body.
By testing a number of combinations of heads, tails and linkers, as well as other parts of the LNPs such as polyethylene or glycol cholesterol, the scientists have been able to target not only the brain or immune system but also the liver, spleen and even definite cell types.
The two principal lung-targeting LNPs, 306-N16B and 113-N16B — both had linkers comprising a nitrogen atom, which appeared to be the solution for targeting the lungs.
We found out that the molecules making up the LNPs would pick up proteins and other molecules from the plasma, and it is that ‘crown’ of material that interacts with the target tissue, organ or cell.
Qiaobing Xu, Study Corresponding Author and Professor of Biomedical Engineering, Tufts University
By examining which plasma proteins adhered to the LNPs, the scientists narrowed it down to 14 proteins as probably having a role in assisting them to adhere to and absorb into the lungs, including albumin, ApoE, fibrinogen beta and fibrinogen gamma.
“It does become a trial and error process to find the right targeting combination, but we can definitely find that combination within a time frame needed for discovering treatments of a wide range of diseases.”