Scientists from the University of Michigan's Rogel Cancer Center were hopeful when they discovered a tiny molecule that obstructed an important pathway in brain tumors. However, there was an issue: they were unsure of how to transport the inhibitor via the bloodstream and into the brain to make contact with the tumor
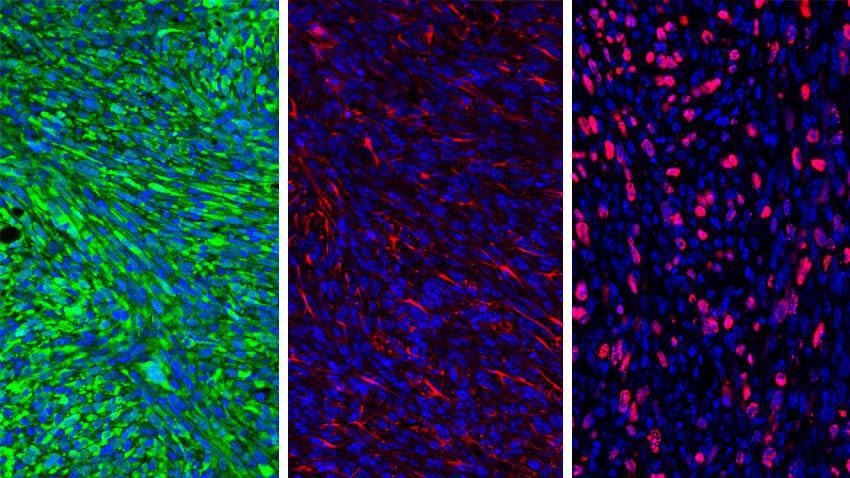 Glioma cells. Image Credit: University of Michigan Rogel Cancer Center
Glioma cells. Image Credit: University of Michigan Rogel Cancer Center
In partnership with many labs, the researchers created a nanoparticle to hold the inhibitor, and the outcomes were even better than anticipated.
The nanoparticles not only transported the inhibitor to the tumor in mouse models, where the drug effectively turned on the immune system to destroy the cancer, but also activated the immune memory via the process so that a reintroduced tumor was removed — an indication that this potential new method could treat brain tumors as well as delay or prevent relapses.
No one could get this molecule into the brain. It’s really a huge milestone. Outcomes for patients with glioma have not improved for the last 30 years.
Maria G. Castro, Ph.D., R.C. Senior Study Author and Schneider Collegiate Professor of Neurosurgery, Michigan Medicine
The study has been published in the journal ACS Nano.
Despite survival gains in many cancer types, glioma remains stubbornly challenging, with only 5% of patients living five years after their diagnosis.
Pedro R. Lowenstein, M.D., Ph.D., Study Author and Richard C. Schneider Collegiate Professor of Neurosurgery, Michigan Medicine
Gliomas are frequently resistant to conventional therapies, and the environment within the tumor overpowers the immune system, causing new immune-based therapies to be unproductive. Plus, there is the challenge of crossing the blood–brain barrier, and it becomes even more cumbersome to deliver functional treatments to these tumors.
The Castro-Lowenstein lab saw an opening. The small molecule inhibitor AMD3100 was created to obstruct the action of CXCR12, a cytokine discharged by the glioma cells which forms a buffer around the immune system, stopping it from firing up against the invasive tumor.
The scientists demonstrated in mouse models of glioma that AMD3100 stopped CXCR12 from attaching to immune-suppressive myeloid cells. By demobilizing these cells, the immune system stays intact and can destroy the tumor cells.
However, AMD3100 was unable to reach the tumor. The drug did not flow well via the bloodstream, and it did not cross the blood–brain barrier, a crucial issue with transporting drugs into the brain.
The Castro-Lowenstein lab worked together with Joerg Lahann, Ph.D., Wolfgang Pauli Collegiate Professor of Chemical Engineering at the U-M College of Engineering, to develop protein-centered nanoparticles to enclose the inhibitor, in the hope of helping it travel via the bloodstream.
Castro is also associated with Anuska V. Andjelkovic, M.D., Ph.D., professor of pathology and research professor of neurosurgery at Michigan Medicine, whose work focuses on the blood–brain barrier. They discovered that glioma tumors form abnormal blood vessels which obstruct regular blood flow.
The scientists administered the AMD3100-loaded nanoparticles as an injection into mice with gliomas. The nanoparticles held a peptide on the surface that attaches to a protein typically found on the brain tumor cells.
As the nanoparticles moved via the bloodstream to reach the tumor, they discharged AMD3100, which reestablished the functionality of the blood vessels. The nanoparticles could then make contact with their target, where they discharged the drug, thus hindering the invasion of the immune-suppressive myeloid cells into the tumor mass. This enabled the immune cells to destroy the tumor and delay its development.
If you don’t have blood flow, nothing will get to your target. That’s why tumors are so smart. But AMD3100 restores the conduits, which is what allows the nanoparticles to reach the tumor.
Maria G. Castro, Ph.D., R.C. Senior Study Author and Schneider Collegiate Professor of Neurosurgery, Michigan Medicine
Additional studies in mice and patient cell lines showed that coupling the AMD3100 nanoparticle with radiation therapy improved the effect beyond either only the nanoparticle or radiation.
Among the mice whose tumors were destroyed, the team then reintroduced the tumor, mimicking a relapse. Without requiring any extra therapy, 60% of mice stayed cancer-free. This indicates that similar to a vaccine, AMD3100 formed immune memory, allowing the immune system to detect and kill the reintroduced cells. While it stopped a relapse in mice, Castro explains it bodes well for at least delaying relapse in humans.
Every glioma recurs. It’s very important for glioma therapy to have this immunological memory.
Maria G. Castro, Ph.D., R.C. Senior Study Author and Schneider Collegiate Professor of Neurosurgery, Michigan Medicine
Preliminary tests revealed little to zero impact on kidney, liver, or heart function and regular blood counts in the mice after treatment. The nanoparticle has an analogous base to ones that have previously been tested in humans and established to be safe. Supplementary safety testing is needed prior to moving to a clinical trial phase.
Funding for this work was provided by the National Institutes of Health grants R37-NS094804, R01-NS105556, R01-NS122536, R01-NS124167, R21-NS123879-01, R37-NS094804, R01-NS105556, R01-NS122536, R01-NS124167, R21-NS123879-01, T32-CA009676, F31CA247104, F31CA247104; Rogel Cancer Center; Michigan Medicine Department of Neurosurgery; Pediatric Brain Tumor Foundation; Leah’s Happy Hearts Foundation; Ian’s Friends Foundation; Chad Tough Foundation; Smiles for Sophie Forever Foundation; Agencia Nacional de Promocion Cientifica y Tecnologica, Argentina; Instituto Nacional del Cancer Argentina, Asistencia Financiera IV.
Journal Reference:
Alghamri, M. S., et al. (2022) Systemic Delivery of an Adjuvant CXCR4–CXCL12 Signaling Inhibitor Encapsulated in Synthetic Protein Nanoparticles for Glioma Immunotherapy. ACS Nano. doi.org/10.1021/acsnano.1c07492.