May 23 2017
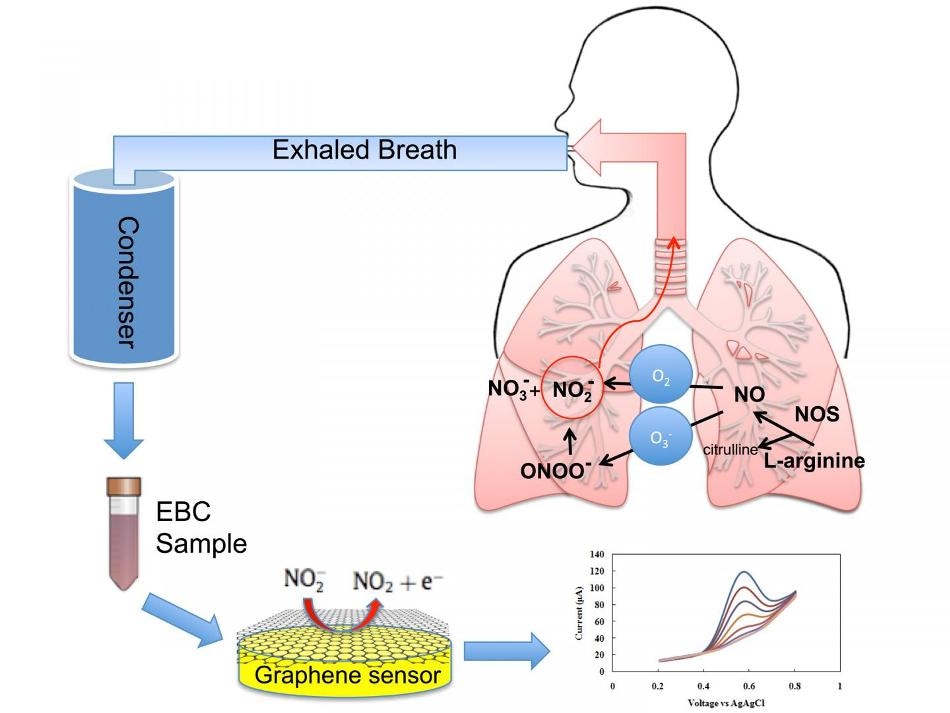 Exhaled breath condensate (tiny droplets of liquid) are rapidly analyzed by a graphene-based nanoelectronic sensor that detects nitrite, a key inflammatory marker in the inner lining of the respiratory airway. (Photo: Azam Gholizadeh)
Exhaled breath condensate (tiny droplets of liquid) are rapidly analyzed by a graphene-based nanoelectronic sensor that detects nitrite, a key inflammatory marker in the inner lining of the respiratory airway. (Photo: Azam Gholizadeh)
Rutgers University-New Brunswick researchers have developed a graphene-based sensor that could pave the way towards earlier detection of looming asthma attacks and enhance the management of asthma and other respiratory diseases, thus preventing hospitalizations and fatalities.
The sensor will aid in the development of devices – possibly similar to fitness trackers like the Fitbit – which patients could wear and then be aware of when and at what dosage to take their medication.
Our vision is to develop a device that someone with asthma or another respiratory disease can wear around their neck or on their wrist and blow into it periodically to predict the onset of an asthma attack or other problems. It advances the field of personalized and precision medicine.
Mehdi Javanmard, Assistant Professor, Department of Electrical and Computer Engineering, Rutgers University
Javanmard and a diverse team of Rutgers-New Brunswick researchers provide details of their invention in a study published online today in the Microsystems & Nanoengineering journal.
Asthma, which causes inflammation of the airway and blocks air flow, affects approximately 300 million people around the world. In 2014, nearly 17.7 million adults and 6.3 million children in the U.S were diagnosed with asthma. Symptoms include coughing, shortness of breath, wheezing, and chest tightness. Other serious lung diseases include chronic obstructive pulmonary disease (COPD), which encompasses chronic bronchitis and emphysema.
Today’s non-invasive techniques for diagnosing and monitoring asthma are inadequate in characterizing the degree and nature of airway inflammation, and require expensive, bulky equipment that patients cannot easily carry with them. The techniques include spirometry, which tests for exhaled nitric oxide, an indicator of airway inflammation, and measures breathing capacity. There is an urgent necessity for enhanced, minimally invasive techniques for the molecular diagnosis and monitoring of asthma, the research says.
By measuring biomarkers in exhaled breath condensate – small liquid droplets released during breathing, doctors can understand asthma at the molecular level, which can then result in targeted treatment and improved disease management.
The miniaturized electrochemical sensor built by the team accurately measures nitrite in exhaled breath condensate using reduced graphene oxide. Reduced graphene oxide is capable of resisting corrosion, has excellent electrical properties, and is highly accurate in detecting biomarkers. Graphene is basically a thin layer of the graphite used in pencils.
Nitrite level in breath condensate is a promising biomarker for inflammation in the respiratory tract. Having a rapid, easy method to measure it can help an asthmatic determine if air pollutants are affecting them so they can better manage use of medication and physical activity. It could also be used in a physician’s office and emergency departments to monitor the effectiveness of various anti-inflammatory drugs to optimize treatment.
Clifford Weisel, Professor, Environmental and Occupational Health Sciences Institute, Rutgers University
“Increases in airway inflammation may be an early warning sign of increased risk of an asthma attack or exacerbation of COPD, allowing for earlier and more-effective preventive measures or treatment,” said Robert Laumbach, study co-author and an occupational and environmental medicine physician at EOHSI.
Just looking at coughing, wheezing and other outward symptoms, diagnosis accuracy is often poor, so that’s why this idea of monitoring biomarkers continuously can result in a paradigm shift. The ability to perform label-free quantification of nitrite content in exhaled breath condensate in a single step without any sample pre-treatment resolves a key bottleneck to enabling portable asthma management.
Mehdi Javanmard, Assistant Professor, Department of Electrical and Computer Engineering, Rutgers University
The following step is to build a portable, wearable system, which could be available in the market within five years, he said. The researchers also aim to expand the quantity of inflammation biomarkers a device could detect and measure.
“In the U.S. alone, allergy inflammation, asthma and various respiratory conditions are all on the rise, so devices that can help diagnose, monitor and manage these conditions will be in high demand,” Javanmard said.
The lead author of the study is Azam Gholizadeh, a doctoral student in the Department of Electrical and Computer Engineering at Rutgers. Other authors include Damien Voiry, a former Rutgers post-doctoral associate in the Department of Materials Science and Engineering who is now at the University of Montpellier in France; Andrew Gow of the Ernest Mario School of Pharmacy at Rutgers; Howard Kipen of EOHSI; and Manish Chhowalla of the Department of Materials Science and Engineering.