Aug 22 2017
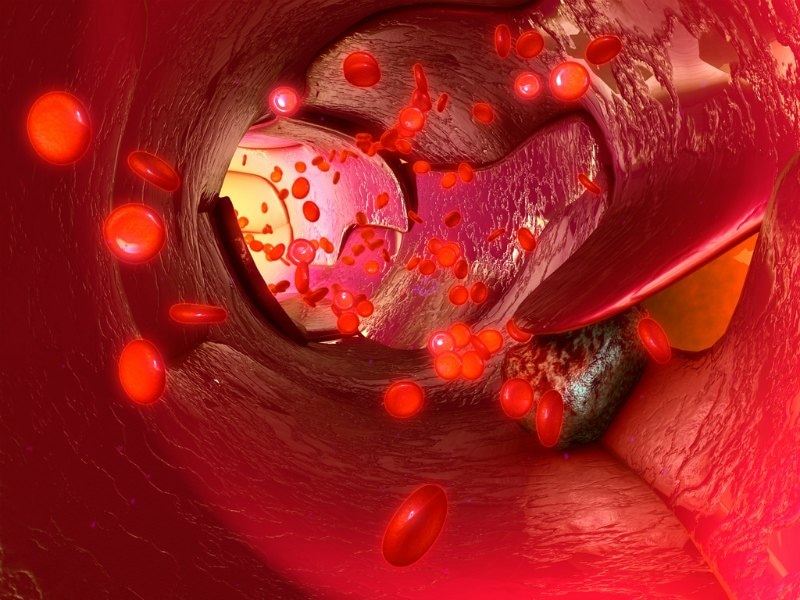
According to a new research work, a nanolaser called the spaser is capable of acting as a water-soluble, super-bright, biocompatible probe that has the potential to find metastasized cancer cells in the blood stream and then kills these cells.
 Credit: Georgia State University
Credit: Georgia State University
From the research, it was clear that the spaser could be used as an optical probe and when discharged into the body (possibly via an injection or drinking a solution), it can locate and target circulating tumor cells (CTCs), stick to them and then destroy these cells by breaking them apart in order to prevent cancer metastases. The spaser, after absorbing laser light, heats up, generates shock waves in the cell and eventually destroys the cell membrane. These findings can be found in the Nature Communications journal.
The spaser represents surface plasmon amplification by stimulated emission of radiation. It is a nanoparticle that is about 20 nm in size or hundreds of times smaller than human cells. As it has folic acid attached to its surface, selective molecular targeting of cancer cells is possible. Usually overexpressed on the surface of most human cancer cells, the folate receptor is poorly expressed in normal cells.
This discovery was brought about by Scientists at Georgia State University, the University of Arkansas for Medical Sciences, the University of Arkansas at Little Rock and the Siberian Branch of the Russian Academy of Science.
There is no other method to reliably detect and destroy CTCs. This is the first. This biocompatible spaser can go after these cells and destroy them without killing or damaging healthy cells. Any other chemistry would damage and likely kill healthy cells. Our findings could play a pivotal role in providing a better, life-saving treatment option for cancer patients.
Dr. Mark Stockman, Director of the Center for Nano-Optics and Professor of Physics, Georgia State
A process called metastasis leads to metastatic cancer, in which cancer spreads to distant parts of the body, typically to the liver, lungs, bone and brain. This is referred to as stage IV cancer by different types of cancers. According to the National Institute of Health’s National Cancer Institute, it can be really hard to control the cancer as soon as it spreads, and unfortunately current treatments are incapable of curing a majority of the metastatic cancers. CTCs are one of the most dangerous ways through which metastasizing occurs and this research is aimed at detecting and destroying CTCs using spasers.
The spasers used in this work were capable of measuring only 22 nm, setting the record for the tiniest nanolasers. A nanometer is one-billionth of a meter. A majority of the results were acquired with a spherical, gold nanoparticle surrounded by a silica shell and covered with a uranine dye, which is extensively used for biomedical and tracing diagnostics.
The Scientists analyzed the capabilities of the spaser in vitro in human breast cancer cells with high folate receptor expression and endothelial cells with low folate receptor expression, and also in mouse cells in vivo.
It was observed that cells with spasers showed high image contrasts with one or many individual “hot spots” at varied laser energies beyond the spasing threshold. Many electron and optical microscopy techniques confirmed the presence of spasers, thus revealing an initial accumulation of individual spasers on the cell membrane which was then followed by their entrance into the cell cytoplasm.
In addition, the research also found that the spacers were less toxic for human cells. At the same time, the spasers exposed to laser irradiation selectively killed the tumor cells without affecting the healthy ones.
The results obtained from the study highlight that spaser-based therapeutic applications with high-contrast imaging are a promising field. The data proposed that spasers have high potential as diagnostic and therapeutic agents that are capable of incorporating optical diagnosis and photothermal-based cell killing, using only a few laser pulses in order to kill cancer cells.
The National Institutes of Health, the National Science Foundation, the University of Arkansas for Medical Sciences and the U.S. Office of Naval Research funded this research.