Venous abnormalities, comprising tissues primarily composed of abnormally shaped veins, can pose significant challenges for treatment, particularly when situated in sensitive areas such as the eyes, face, and genitourinary organs.
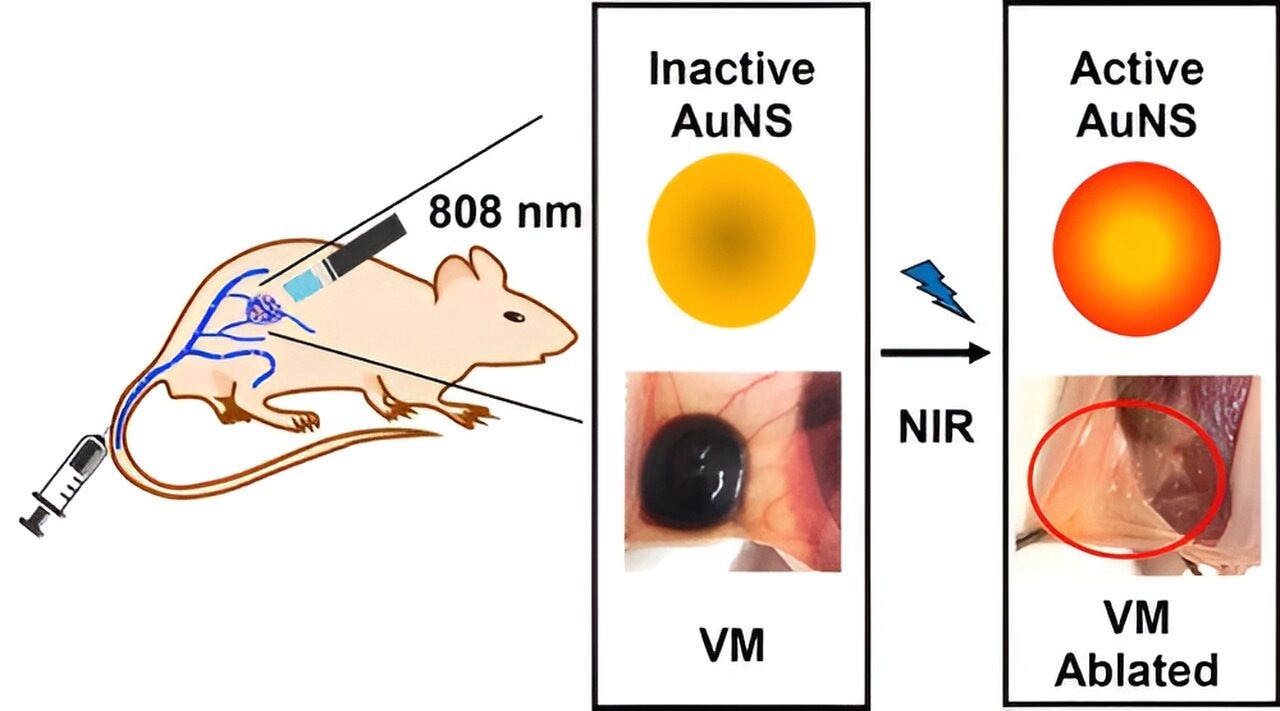
Image Credit: Nano Letters.
In severe cases, these lesions can be disfiguring and may lead to the compression or obstruction of surrounding tissues. They can also cause bleeding and clotting, interfere with breathing or vision, and impair circulation.
Katie Ladlie, aged 25, has experienced the challenges associated with venous abnormalities. The lesions have affected various parts of her body, with the most significant impact on her left leg. In her childhood, she sought treatment at the Vascular Anomalies Center at Boston Children's Hospital, traveling from Missouri for multiple treatments.
While these treatments were effective in managing some of her smaller lesions, her left leg continued to worsen. The abnormal veins in her leg became enlarged, leading to pain as blood pooled and damaged her knee joint.
Ultimately, as her condition worsened, Katie Ladlie reached a point where she could no longer walk, and traditional treatment options were exhausted. At the age of 12, with a desire to engage in sports and regain mobility, she made the decision to undergo the amputation of her leg at her local hospital in Missouri. The use of a prosthesis offered her the opportunity to lead a more active and mobile lifestyle.
Creating A New Solution For Venous Malformations
Due to the risk of hemorrhage, surgical treatment is often not a safe option for malformations like Katie Ladlie’s. Sclerotherapy, a procedure that involves injecting a solution into the blood vessels to shrink them, proved helpful for some of Ladlie’s smaller lesions.
However, it can be technically challenging, may lead to bleeding, and is not always highly effective, according to Dr. Steven Fishman, who co-directs the Vascular Anomalies Center and was one of Ladlie’s original doctors. Additionally, the available medications can only halt the growth of malformations, often come with side effects, and require indefinite use.
Cases like Katie Ladlie’s have motivated researchers at Boston Children’s Hospital to continue their quest for innovative solutions. One such solution, recently detailed in the journal Nano Letters, holds particular promise.
Many years ago, Pediatric Intensivist and Anesthesiologist Dr. Daniel S. Kohane, MD, Ph.D., and his then-fellow Dr. Kathleen ‘Kate’ Cullion, MD, Ph.D., encountered a teen in the ICU with a severe, basketball-sized venous malformation affecting her thigh and leg. Dr. Kohane, who directs the Laboratory for Biomaterials and Drug Delivery (LBDD) at the hospital, and Dr. Cullion were inspired by a second patient diagnosed with a lymphatic malformation. This patient underwent a contrast dye study aimed at enhancing the visualization of the vessels, sparking the idea of a new method.
“The dye was still in the malformation two months after the study,” recounts Dr. Kohane. “The dye was made up of nanoparticles that zip through normal blood vessels. But the abnormal vessels were leaky, and the particles accumulated there. Kate and I said, 'I wonder if the same thing would happen with venous malformations.'"
The researchers hypothesized that the propensity for drugs to diffuse out of malformed and leaky vessels into surrounding tissues could be leveraged to accumulate the drug precisely where it is needed. This approach enhances efficacy, permitting higher doses while preventing off-target effects in other parts of the body.
Nanoparticles Plus Phototherapy Shrink Malformations
To test their hypothesis, Dr. Kohane and Dr. Cullion utilized mice with bioengineered networks of human vessels that mimicked venous malformations. These engineered vessels were developed in the lab of Dr. Juan Melero-Martin, Ph.D. The researchers administered intravenous injections of nanoparticles to the mice and monitored the distribution of the particles within the body.
We proved that you could get nanoparticles to preferentially accumulate in the anomalous vessels.
Kohane, Cullion, Assistant Director, Laboratory for Biomaterials and Drug Delivery, Boston Children's Hospital
In their recent study, the researchers examined a nanoparticle-based photothermal therapy using a mouse model of venous malformations. Initially, they intravenously injected the mice with gold nanoparticles, which gathered in the malformations.
Subsequently, they exposed the nanoparticle-filled lesions to near-infrared light. The irradiated gold particles produced heat, leading to a significant reduction in the malformations and, in some cases, complete elimination.
Dr. Kohane was blown away. “The mice had some venous malformations twice the diameter of a pea and two days later there was nothing.”
A First-In-Human Trial?
Dr. Kohane, Dr. Cullion, and Surgical Fellow Dr. Claire Ostertag-Hill, MD, have filed for a patent on the technology using the proof of principle and early evidence of safety—the first use of nanomedicine to treat vascular anomalies. Dr. Kohane envisions that this approach could transition to clinical use relatively swiftly, particularly because there are already ongoing clinical trials employing a similar approach in cancer treatment.
I think this treatment will be great for more complex vascular anomalies, or those in difficult locations. Large anomalies might require several treatments, but at the very least this approach could shrink them and make surgery less risky. In very complex patients, it could be used in conjunction with other procedures.
Claire Ostertag-Hill, Boston Children's Hospital
Dr. Fishman, in his role as surgeon-in-chief, has actively directed fellows toward the Kohane lab and fully endorses the progression of this initiative.. “As soon as they have further validation in animals and institutional and regulatory approval, we have plenty of patients who would sign up to be the first human treated, because they have no other good options or other options have failed. This work is innovative and will hopefully make a difference,” he notes.
Katie Ladlie is optimistic about the research as well. Currently, she actively participates in the US Women's Sled Hockey team, maneuvering low on the ice with hockey sticks serving as ice picks. In addition to her sports involvement, she has taken on a new role at Spaulding Rehabilitation Hospital, where she facilitates adaptive sports opportunities for individuals with disabilities.
Katie Ladlie consults doctors at Boston Children’s, though she is an adult now, because of their wide knowledge of vascular anomalies. She says, “I am so excited with all the new research and education that has been coming out with venous malformations.”
Journal Reference:
Cullion, K. et al. (2023) ‘Ablation of venous malformations by photothermal therapy with intravenous gold Nanoshells’, Nano Letters, 23(15), pp. 7092–7099. doi:10.1021/acs.nanolett.3c01945.