Jan 19 2011
With an invention that can be made from some of the same parts used in CD players, University of Michigan researchers have developed a way to measure the growth and drug susceptibility of individual bacterial cells without the use of a microscope.
The new biosensor promises to speed treatment of bacterial infections, said Raoul Kopelman, who is the Richard Smalley Distinguished University Professor of Chemistry, Physics and Applied Physics and a professor of biomedical engineering, biophysics and chemical biology.
 The U-M group demonstrated that the sensor not only can monitor the growth of a single bacterium throughout its life cycle and over multiple generations, but it can also determine when an individual bacterium stops growing, in response to treatment with an antibacterial drug, for instance.
The U-M group demonstrated that the sensor not only can monitor the growth of a single bacterium throughout its life cycle and over multiple generations, but it can also determine when an individual bacterium stops growing, in response to treatment with an antibacterial drug, for instance.
Instead of waiting days for culture results, clinicians will be able to determine in minutes the antibiotic best able to treat the infection. This advance, along with the sensor's potential use in screening existing and newly discovered compounds for antibiotic activity, could improve patient outcome, reduce healthcare costs and reduce the spread of antibiotic resistance
Because it also detects the response of individual cancer cells, the sensor could someday be used as well in cancer drug development and treatment. The research is reported in the Jan. 15 issue of the journal Biosensors and Bioelectronics.
The device, called an asynchronous magnetic bead rotation (AMBR) sensor, was invented in Kopelman's lab at U-M. Early development of the sensor, also in the Kopelman lab, was primarily the work of Brandon McNaughton, who was a graduate student at the time. McNaughton went on to found the U-M spinoff Life Magnetics Inc., where as chief technological officer he is further developing the device.
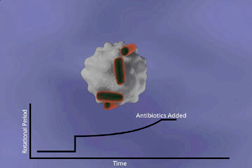
The AMBR sensor uses a spherical, magnetic bead that asynchronously spins in a magnetic field. Just as a pencil attached to a child's toy top creates drag that affects the way the top spins, anything attached to the bead slows its rate of rotation. In the current work, the researchers attached individual, rod-shaped Escherichia coli bacteria to individual beads and watched what happened, using the newly developed AMBR sensor.
"When one bacterium gets attached, it's hanging out there like a little hotdog, and it changes the drag tremendously, slowing down the rate of rotation by a factor of four," said Kopelman. "If the bacterium grows even a tiny bit, the drag increases even more, and we can monitor that nano-growth by observing changes in the rate of rotation."
"The method can detect growth of as little as 80 nanometers, making it far more sensitive than even a powerful optical microscope, which has a resolution limit of about 250 nanometers," said graduate student Paivo Kinnunen, one of the paper's lead authors, who is
also working at Life Magnetics while completing his studies. (While the AMBR sensor does not require a microscope, one was used in the current study to confirm results).
The U-M group demonstrated that the sensor not only can monitor the growth of a single bacterium throughout its life cycle and over multiple generations, but it can also determine when an individual bacterium stops growing, in response to treatment with an antibacterial drug, for instance.
"You can basically tell, within minutes, whether or not the antibiotic is working," said Kinnunen.
In the near future, "we expect it will be possible to make the determination even quicker," said graduate student Irene Sinn, the paper's other lead author. "This is something we are actively working on."
The device also can be used for monitoring the growth and drug susceptibility of other types of cells, said Kinnunen. "The sensor is very sensitive to small changes in growth, so this method can be applied to any applications in the microscale or nanoscale where there are small changes in size. That includes the growth of yeast and cancer cells as well as bacteria."
The technology could have far-reaching implications, said McNaughton.
"At Life Magnetics we are very excited and optimistic about leveraging the single cell sensitivity of the AMBR technology to develop a product that will determine the best antimicrobial in hours instead of days," he said. "This will have a dramatic positive impact for patients and for the health system, cutting costs and saving lives. Inappropriate therapy and the overuse of antimicrobials are large contributors to the problem of increased resistance in bacteria. In fact, with superbugs such as MRSA causing every year in the U.S. more deaths than HIV/AIDS, it is no surprise that the Centers for Disease Control and Prevention considers antimicrobial resistance to be among the most pressing health problems. Our technology is designed to attack that problem."
Source: http://www.umich.edu/