Oct 19 2013
Manchester Cancer Research Centre (MCRC) scientists have taken delivery of three new sophisticated research tools thanks to funding from the HEFCE UK Research Partnership Investment Fund (UKRPIF).
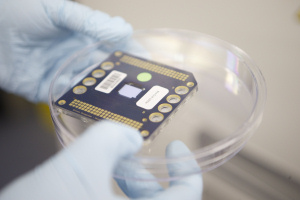 New MCRC equipment
New MCRC equipment
The University of Manchester secured £12.8 million from UKRPIF to part-fund the construction of the new research centre for the MCRC, a partnership between The University, Cancer Research UK and The Christie NHS Foundation Trust, and to pay for vital equipment.
The specialised instruments will provide the platform technologies necessary to implement personalised medicine for cancer patients in the North West. MCRC scientists will be able to use the new equipment to get the most information possible from cancer and normal cells and a fuller picture of the processes and mechanisms that drive cancer.
The HiSeq Next Generation Sequencing machine can be used to sequence entire genomes (all the genetic information in a cell), or selectively sequencing areas of the genome that code for proteins (the exome).
The advantage of exome analysis over whole genome sequencing is that it represents around 1.5% of the entire genome. This drastically reduces the amount of sequence data that is needed, thereby reducing the cost. The high throughput of the HiSeq can generate 50-fold coverage of four complete human genomes in under two weeks, equivalent to 120Gb of data in just over a day.
Genetic information held in DNA is first transcribed into RNA (RNA transcripts) before being translated into functional proteins. MCRC scientists will also be using the new equipment to sequence transcriptomes – a collection of all the transcripts present in a given cell
By studying transcriptomes, MCRC scientists will be able to determine when and where each gene is active or inactive in specific cells and tissues. They will also be able to define the level of activity for each gene. “Nearly all cells in the human body have the same genes but show different patterns of activity or gene expression: these differences are responsible for how cells behave. By comparing transcriptomes from cancer cells and normal cells, we will get a better understanding of the differences in gene expression that contribute to cancer development and progression,” explained MCRC’s Dr Ged Brady, Senior Translational Scientist at the Paterson Institute for Cancer Research.
A major research focus within the MCRC is using circulating tumour cells (CTCs) to get information about the activity and status of the tumour, especially in tumours like lung cancer where a biopsy may not be possible. However, isolating the few CTCs that may be present among thousands of normal blood cells can be a challenge. Using the DEPArray, individual cancer cells can be gently trapped in ‘electronic cages’ using electrostatic plates and each cell collected using a ‘drag and drop’ technique to isolate rare cells or specific cell populations. The DEPArray has special image analysis software that enables visual inspection of trapped cells so that scientists can ensure they select only the cells of interest for further analysis.
Identifying and understanding genetic differences between cancer cells and normal cells, and between the same types of cancer in different individuals, is key to developing personalised treatments for patients. ImageStreamX not only sorts cells but takes an electronic picture of each one as it passes a detector – allowing visualisation of any differences and variations. Each cell can be labelled with up to eight different fluorescent dyes, which detect specific proteins. Using this technology, scientists can see how much of each protein is present, where it is located and how it relates to other proteins in the cell.
This protein-protein relationship is critically important in dictating how the cell behaves. For example, a cancer drug could need several proteins working together to be effective – some to transport the drug into the cell and others to mediate drug activity. Identifying key proteins and their relationships helps MCRC scientists to understand important processes such as drug resistance mechanisms, and to assess why some cancers respond to certain treatments while others don’t.
Dr Gerard Brady, from Manchester Cancer Research Centre part of The University of Manchester, said: “With thousands of patients taking part in clinical trials at The Christie every year and donating blood and tumour samples, the new equipment means that we can maximise the amount of information we get from each sample. We will be able to provide a fuller picture of each cancer and individual variations, which we can use to eventually improve treatments and patient outcomes."