Apr 10 2014
Synthetic collagen invented at Rice University may help wounds heal by directing the natural clotting of blood.
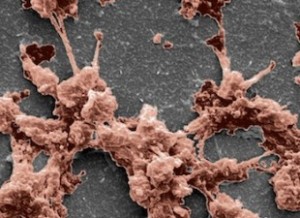 Clumping platelets, seen in an electron microscope image, demonstrate the clotting and healing power of a synthetic hydrogel created at Rice. Courtesy of the Hartgerink Group
Clumping platelets, seen in an electron microscope image, demonstrate the clotting and healing power of a synthetic hydrogel created at Rice. Courtesy of the Hartgerink Group
The material, KOD, mimics natural collagen, a fibrous protein that binds cells together into organs and tissues. It could improve upon commercial sponges or therapies based on naturally derived porcine or bovine-derived collagen now used to aid healing during or after surgery.
The lab of Jeffrey Hartgerink, a chemist and bioengineer based at Rice's BioScience Research Collaborative, developed synthetic collagen several years ago. The lab's analysis of KOD for use as a hemostat, or clotting agent, appears this month in the American Chemical Society journal Biomacromolecules.
Hartgerink and lead author Vivek Kumar, a postdoctoral researcher at Rice, viewed clotting as a good avenue of investigation for practical application of KOD, a synthetic protein made of 36 amino acids that self-assemble into triple-helix nanofibers and hydrogels.
"We showed we can make small peptides that we can easily synthesize chemically, which means we can purify them for a completely homogeneous material," Hartgerink said. "Those peptides self-assemble into fibers that in turn become a hydrogel. This hierarchy of assembly — from a peptide to a triple helix to a fiber to a hydrogel — mimics much of the hierarchy of assembly of natural collagen."
Hartgerink said collagen's importance goes beyond its role as a scaffold for cells. "How a cell determines what it's going to do depends in large part on the chemical surface it's attached to," he said.
"We've been thinking about KOD for hemostasis for a long time. Natural collagen is already used in a variety of on-the-market products for hemostasis, but there are benefits to a synthetic system. We can avoid the immune problems associated with using collagen from cows, for example. The ability to synthesize KOD chemically gives us a pure product."
Lab tests showed KOD hydrogel traps red blood cells to stop bleeding and, unlike commercial barriers, binds and activates platelets that form clots to promote healing. The tests also determined KOD does not promote inflammation.
"We wouldn't envision using KOD for major trauma, because there are conventional methods like tourniquets or using clay-based materials that are much more effective in that immediate situation," said Kumar, who often used his own blood to test the hydrogel against commercial hemostats. "We see using this for more specific, site-directed applications, like to stop surgical bleeding."
"This is not going to be a battlefield dressing or something a first responder is likely to use," Hartgerink said. "But when the goal is to promote delicate and natural healing where scarring is a concern, this can be more nuanced and effective."
While validation is needed for KOD to be used in operating rooms, the researchers are already considering applications for wound healing and graft support. "We have the flexibility to incorporate higher levels of complexity within our peptide matrix," Kumar said. "We can incorporate cell adhesion or degradation sites to recruit cells or draw in different components from native tissue."