Nov 26 2014
A new hybrid vehicle is under development.
Its performance isn’t measured by the distance it travels, but rather the delivery of its cargo: vaccines that contain genetically engineered DNA to fight HIV, cancer, influenza and other maladies.
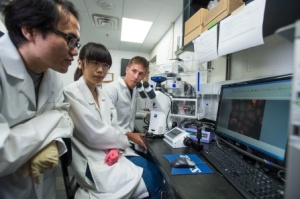 University at Buffalo researchers, including Charles Jones, far right, a doctoral candidate in the Department of Chemical and Biological Engineering, are developing new technology to improve DNA vaccines. Credit: Onion Studio.
University at Buffalo researchers, including Charles Jones, far right, a doctoral candidate in the Department of Chemical and Biological Engineering, are developing new technology to improve DNA vaccines. Credit: Onion Studio.
Described recently in the Proceedings of the National Academy of Sciences, the technology is a biomedical advancement that could help unleash the potential of DNA vaccines, which despite two decades of research, have yet to make a significant impact in the treatment of major illnesses.
“The technology that we’re developing could help take immunization to the next level,” said Blaine A. Pfeifer, PhD, an associate professor in the Department of Chemical and Biological Engineering in the School of Engineering and Applied Sciences at the University at Buffalo.
Pfeifer, the study’s lead author, added: “By improving the delivery of DNA vaccines, we can potentially harness the human immune system in new ways to fight everything from the flu and herpes to HIV and cancer.”
Conventional vaccines, like those used to fight polio and smallpox, are typically composed of an agent that contains weakened or killed forms of the disease-causing microbe. The agent prompts the immune system to recognize the agent as foreign, destroy it, and keep a record of it so the immune system can more effectively fight it in the future.
While effective, some vaccines don’t last, others can revert to dangerous forms and some are costly and time-consuming to develop. Furthermore, no effective vaccines exist for cancer, malaria and others diseases that kill millions of people worldwide annually.
DNA vaccines could address these problems.
To create them, researchers analyze disease-causing sources, such as a pathogenic microbe. They then isolate copies of the microbe’s genes (usually one or two) responsible for the disease.
The genetically engineered DNA is injected into the body, whereupon being processed by the immune cells, directs the production and presentation of antigens which provoke an adaptive immune response capable of destroying the disease.
Essentially, the body’s own cells become vaccine-making factories that create the antigens necessary to stimulate the immune system, according to the National Institute of Allergy and Infectious Diseases.
In theory, DNA vaccines can generate broad immune responses; they are relatively inexpensive to create; and they can’t cause the disease because they don’t contain the source of the disease, only a few of its genes. Dozens of clinical trials involving DNA vaccines are underway. Most are investigating treatments for HIV and cancer, while others involve influenza, hepatitis B and C, HPV and malaria.
A problem limiting the effectiveness of some DNA vaccines, however, is that they do not sufficiently stimulate the immune system. Scientists say this is due, in part, to the inefficient delivery of the genes. For example, some travel to the wrong place while others get caught in intracellular traffic jams.
To address the problem, Pfeifer and his students collaborated with Anders Hakansson, PhD, formerly of the UB School of Medicine and Biomedical Sciences, and a senior co-author of the study.
The team combined two delivery vehicles – a bacterial cell and a synthetic polymer – to create a hybrid. Designed to target specific immune cells (antigen-presenting cells) and more efficiently deliver genes to the nucleus of those cells, the hybrid outperformed the two individual delivery vehicles when tested in a mouse model.
“The hybrid provided a synergistic boost in delivery effectiveness due to its dual nature,” said Charles H. Jones, a doctoral candidate in the Department of Chemical and Biological Engineering at UB and the study’s first author. “We also determined that it’s relatively inexpensive to create and flexible in terms of use. The results thus far are very encouraging.”
The team continues to test the vehicle in different models. The goal, Pfeifer said, is to create a vehicle that will be useful for many DNA vaccines.
The research is supported by the National Institutes of Health and by UB’s Arthur A. Schomburg Fellowship Program.