Jul 31 2019
According to a new study, a protein pumped out of certain—but not all—populations of “helper” cells in the brain, known as astrocytes, play a definite role in controlling the formation of connections among neurons required for learning and forming new memories.
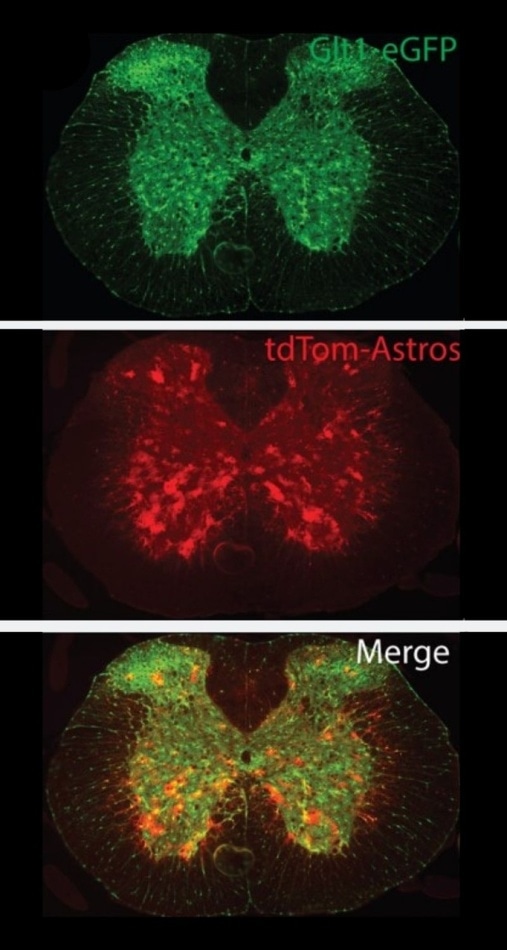 Red 8.3 astrocytes in the spine of a mouse. (Image credit: Rothstein lab)
Red 8.3 astrocytes in the spine of a mouse. (Image credit: Rothstein lab)
This latest evidence was provided by Johns Hopkins Medicine researchers, working with human and mouse tissue.
The researchers used mice that were genetically engineered and bred with fewer such connections, and eventually performed proof-of-concept experiments. These experiments demonstrated that corrective proteins could be delivered through nanoparticles to substitute the missing protein required for “road repairs” on the faulty neural highway.
Considering that these connective networks are either damaged or lost by neurodegenerative diseases, like Alzheimer’s disease or specific types of intellectual disability like Norrie disease, the latest findings can improve efforts to repair and regrow the networks and possibly restore normal brain function, stated the researchers.
The study results have been reported in the May issue of Nature Neuroscience.
We are looking at the fundamental biology of how astrocytes function, but perhaps have discovered a new target for someday intervening in neurodegenerative diseases with novel therapeutics.
Jeffrey Rothstein, MD, PhD, the John W. Griffin Director of the Brain Science Institute and Professor of Neurology, Johns Hopkins University School of Medicine
Rothstein continued, “although astrocytes appear to all look alike in the brain, we had an inkling that they might have specialized roles in the brain due to regional differences in the brain’s function and because of observed changes in certain diseases. The hope is that learning to harness the individual differences in these distinct populations of astrocytes may allow us to direct brain development or even reverse the effects of certain brain conditions, and our current studies have advanced that hope.”
Astrocytes, within the brain, are the support cells that serve as guides to direct fresh cells, clean up byproducts resulting from the metabolism of brain cells, and promote chemical signaling.
A specific astrocyte protein, called glutamate transporter-1, was the target of Rothstein’s team. According to earlier studies, this protein was lost from astrocytes in specific parts of the brains with neurodegenerative diseases.
The protein, similar to a biological vacuum cleaner, usually ingests the chemical “messenger” glutamate from the spaces existing between neurons as soon as a message is delivered to another cell. This step is needed to close the transmission and inhibit the accumulation of toxic levels of glutamate.
When the glutamate transporters vanish from some parts of the brain, like the spinal cord and motor cortex in people suffering from amyotrophic lateral sclerosis (ALS), the glutamate remains around for a much longer time, conveying messages that over-stimulate and destroy the cells.
To understand how the brain decides the types of cells that require the glutamate transporters, Rothstein and team concentrated on the DNA region in front of the gene that normally regulates the on-off switch required to produce the protein. The mice were genetically engineered to glow red in each cell where the gene is stimulated.
The glutamate transporter is usually turned on in all the astrocytes. However, all the cells and neurons in the brain glowed red when the researchers applied 1,000- to 7,000-bit segments of DNA code from the on-off switch for the glutamate transporter.
When the researchers attempted the largest sequence of an 8,300-bit DNA code from this site, they started to observe some selection in the red cells. Such red cells were all astrocytes but only in certain layers of the brain’s cortex in mice.
Since these “8.3 red astrocytes” can be identified, the investigators believed that these cells may have a particular function that is different from other astrocytes present in the brain. To determine the exact function of these 8.3 red astrocytes in the brain, the scientists utilized a cell-sorting machine to isolate the red astrocytes from the uncolored equivalents in the cortical tissue of the mouse brain.
They subsequently identified the type of genes that were turned on to relatively higher than normal levels in the red astrocytes when compared to the uncolored cell populations. The 8.3 red astrocytes were found to turn on elevated levels of a gene that codes for Norrin—a different kind of protein.
Neurons from normal mouse brains were taken and then treated with Norrin. The researchers ultimately discovered that those neurons grew more of the extensions, or “branches”, utilized to send chemical messages among the brain cells.
When the researchers observed the brains of mice that were genetically engineered without Norrin, they found that these neurons had fewer branches when compared to healthy animals that made Norrin, informed Rothstein.
In another series of experiments, the researchers took the DNA code for Norrin as well as the 8,300 “location” DNA, and then organized them into deliverable nanoparticles. When Norrin nanoparticles were injected into the brains of mice engineered to lack Norrin, the neurons of these mice started to rapidly grow several more branches—a process indicating repair to neural networks. These experiments were also repeated with human neurons.
Rothstein observed that Norrin protein mutations, which reduce protein levels in people, can lead to Norrie disease—a rare, genetic disorder that can cause intellectual disability as well as blindness in infancy.
Since the researchers were able to grow new branches for communication, they believe that Norrin can possibly be used for treating certain types of intellectual disabilities, like Norrie disease, in the future.
Next, the scientists are studying whether Norrin will be able to repair connections in the brains of animal models displaying neurodegenerative diseases. Rothstein and Miller have submitted a patent for Norrin in preparation for potential success.
Other authors of the publication are Sean Miller, Thomas Philips, Namho Kim, Raha Dastgheyb, Zhuoxun Chen, Yi-Chun Hsieh, J. Gavin Daigle, Jeannie Chew, Svetlana Vidensky, Jacqueline Pham, Ethan Hughes, Michael Robinson, Rita Sattler, Jung Soo Suk, Dwight Bergles, Norman Haughey, Mikhail Pletnikov and Justin Hanes of Johns Hopkins, and Malika Datta and Raju Tomer of Columbia University.
The study was funded by grants from the National Science Foundation Graduate Fellowship Research Program and the National Institute of Neurological Disorders and Stroke (R01NS092067, R01NS094239).