Glioblastoma (GBM) is a malignant brain cancer in adults with a median survival period of 15 months from the point of diagnosis. Residual tumor cells that remain beyond the margins of every GBM resection are resistant to postsurgical therapy and are the driving force of mortality. These residual tumor cells reach extensive brain tissues, making it difficult for the therapeutics to target the tumor without causing neural damage.
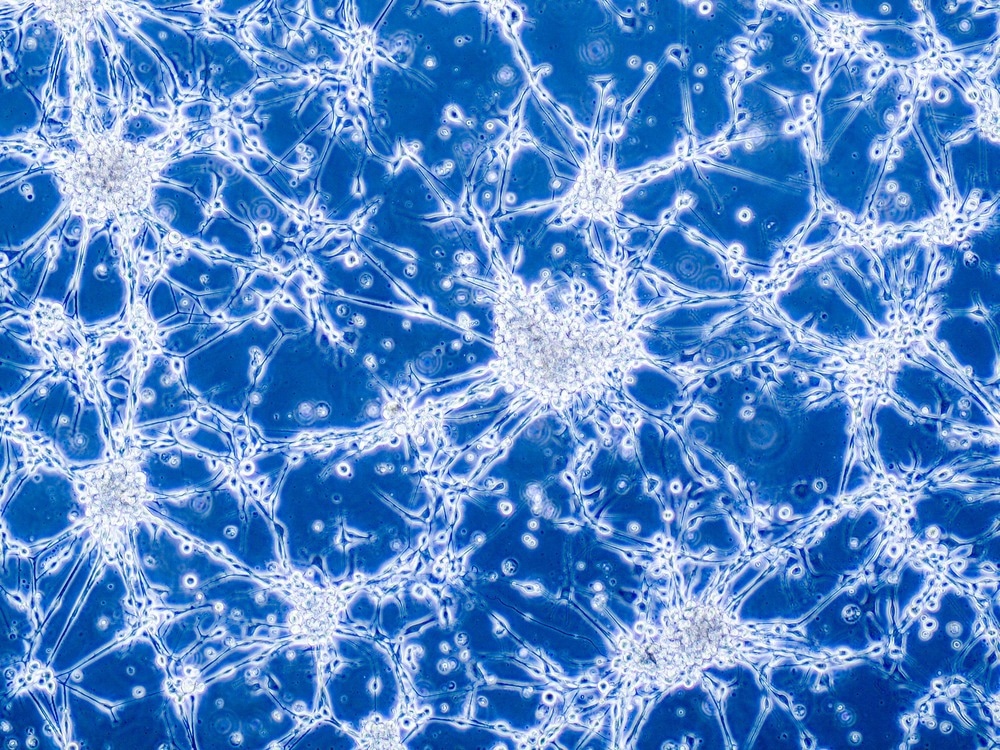
Study: Nanotherapeutic treatment of the invasive glioblastoma tumor microenvironment. Image Credit: Anna Durinikova/Shutterstock.com
Thus, therapeutic development for GBM should either directly target the brain-invading tumor cells or indirectly support invading them and prevent reoccurrence. An article published recently in Advanced Drug Delivery Reviews summarized a few drug delivery techniques and nanotherapeutic technologies. These techniques or technologies target the GBM cells that invade the brain or non-cancerous, invasion-supporting cells that reside within the GBM microenvironment.
Challenges in Treating GBM
GBM is highly heterogeneous, and the stem cell-like glioma cells have infiltrative nature that migrates away from a hypothetical point of origin and reaches extensive brain tissues that are difficult to be treated. Gliomas with areas of necrosis envelope a mass of viable tumor cells that can invade neighboring healthy brain tissue. This invasive nature of GBM retains a few malignant cells even after standard tumor resection leading to recurrence.
The major challenge in GBM treatment is the drug delivery to the tumor site without damaging the surrounding neural cells, as the GBM tumors migrate to deeper brain tissues. Moreover, the presence of the blood-brain barrier (BBB) at the interface of the central nervous system (CNS) and the neurovascular unit (NVU) interrupt the passage of drugs through this BBB membrane resulting in the drug accumulation at a low therapeutic concentration in the brain.
Interstitial and other drug delivery approaches can overcome the BBB transport barrier, effectively delivering therapies more extensively into brain tissues. Furthermore, there have been continuous efforts to investigate these approaches for safety and clinical feasibility. However, target-specific treatments for GBM were clinically unsuccessful.
Nanomedicine Towards GBM Therapy
Nanoparticles (NPs) as drug delivery systems circumvent the drawbacks of conventional chemotherapy. The NPs improve biodistribution and half-life and enhances intracellular accumulation. Moreover, the tunable physicochemical properties and surface profiles are advantageous for tumor-specific targeting.
The controllable drug release kinetics of therapeutic NPs prevents the need for multiple drug administrations. These NPs are also suitable for combination therapy. The NP systems like polymeric NPs, lipid-based NPs, micelles, dendrimers, and inorganic NPs have unique physicochemical and surface properties and were tested preclinically for GBM drug delivery.
The physicochemical properties of NPs majorly determine their feasibility in crossing the BBB and targeting specifically at and into the tumor cells. Previous studies reported on NP diffusion within the brains of rats and humans revealed the favorable characteristics for NP's BBB penetration. The studies confirmed that a pore size distribution between 100 to 200 nanometers, hydrodynamic size of about 100 nanometers, and slightly anionic or neutral surface charge enable NPs to cross BBB.
Clinical NPs in GBM Therapy
Several nanoplatforms are currently under clinical evaluation for either therapy or imaging of brain tumors. These nanotherapeutics are composed of lipids or inorganic materials. Lipid-based NPs are FDA-approved nanomedicines that constitute phospholipids with vesicular structures (unilamellar or multilamellar). These structures facilitate the co-encapsulation of hydrophobic, hydrophilic, and lipophilic drugs within the same liposomal system enabling their application in combination therapy.
Inorganic NPs with intrinsic material properties offer unique physical, magnetic, electrical, and optical properties. Leveraging these unique properties help attain the required features in NPs that otherwise is unachievable via organic or polymeric biomaterials. Inorganic NPs in GBM drug delivery and imaging applications include silica, gold, and iron oxide NPs.
Drug Delivery Strategies Targeting GBM
The BBB neuro-vascular unit is unique, complex, and composed of endothelial cells (ECs). The inter-EC junctions contain proteins joined by a basal lamina and distributed between pericytes and astrocytes.
NPs harness endogenous transport processes like carrier-mediated transcytosis (CMT), receptor-mediated transcytosis (RMT), and adsorptive-mediated transcytosis (AMT). Of the three, the passage of NPs through BBB is better via the RMT-mediated pathway. Moreover, the RMT-mediated transcytosis across the BBB initiates on the brain capillary’s luminal side and microvascular ECs.
The interactions between the NP-based ligand and the receptor trigger continuous trafficking associated with receptor-mediated endocytosis, regulated via vesicles that are either clathrin-decorated or devoid of it and are transported intracellularly to reach multivesicular bodies and finally fuse on the BBB’s abluminal side, which allows the release of trafficking components into brain parenchyma.
Conclusion
To summarize, residual GBM cells, after surgical therapy, invade deeper brain tissues and pose a challenge in GBM patient management. The rapid recurrence of tumors, closer proximity between cancer cells and functional brain cells, and impermeable nature of BBB are primary hindrances to effectively treating GBM-infected cells.
The drug delivery approach based on NPs can eliminate residual glioma cells after surgery. These NPs either can be delivered directly into the brain or can be engineered to cross the BBB via RMT. Moreover, hydrogel-based depot systems and convection-enhanced delivery (CED) can cross the BBB and release drugs locally along the resection cavity.
Reference
Pandey, N., Anastasiadis, P., Carney, C.P., Kanvinde, P.P., Woodworth, G.F., Winkles, J.A. et al. (2022). Nanotherapeutic treatment of the invasive glioblastoma tumor microenvironment, Advanced Drug Delivery Reviews. https://doi.org/10.1016/j.addr.2022.114415
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.